Difference between revisions of "Development of retractable foreskin"
WikiModEn2 (talk | contribs) (→Infants and pre-school: Wikify.) |
WikiModEn2 (talk | contribs) (Add link in SEALSO section.) |
||
| (7 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
{{GraphicWarning}} | {{GraphicWarning}} | ||
| − | [[Image:Side by side retraction.png|right|thumb|A human penis before and after retraction of the foreskin.]] | + | [[Image:Side by side retraction.png|right|thumb|A human [[penis]] before and after retraction of the [[foreskin]].]] |
Infant boys are born with a non-retractable [[foreskin]]. The '''development of retractable foreskin''' occurs gradually over a widely-variable number of years. | Infant boys are born with a non-retractable [[foreskin]]. The '''development of retractable foreskin''' occurs gradually over a widely-variable number of years. | ||
| Line 135: | Line 135: | ||
|date=1996-11-01 | |date=1996-11-01 | ||
|accessdate=2019-10-19 | |accessdate=2019-10-19 | ||
| − | }}</ref> Imamura (1997) examined 4521 infants and young boys. He | + | }}</ref> Imamura (1997) examined 4521 infants and young boys. He reported that the [[foreskin]] is retractile in 3 percent of infants aged one to three months, 19.9 percent of those aged ten to twelve months, and 38.4 percent of three-year-old boys.<ref name="imamura1997">{{REFjournal |
|last=Imamura | |last=Imamura | ||
|init=E | |init=E | ||
| Line 244: | Line 244: | ||
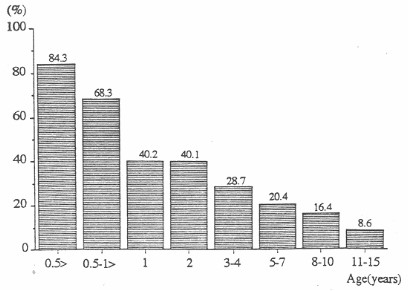
[[File:Kayaba.jpg|left|frame|Percentage of boys with tight ring totally non-retractile foreskin according to Kayaba et al.]]<br clear="all"> | [[File:Kayaba.jpg|left|frame|Percentage of boys with tight ring totally non-retractile foreskin according to Kayaba et al.]]<br clear="all"> | ||
| − | [[Jakob Øster]], a Danish physician who conducted school examinations, reported his findings on the examination of school-boys in [[Denmark]], where [[circumcision]] is rare.<ref name="Øster1968">{{OesterJ 1968}}</ref> Øster (1968) found that the incidence of fusion of the foreskin with the glans penis steadily declines with increasing age and foreskin retractability increases with age.<ref name="Øster1968"/> Kayaba et al. (1996) also investigated the development of foreskin retraction in boys from age 0 to age 15.5 Kayaba et al. also reported increasing retractability with increasing age. Kayaba et al. reported that about only 42 percent of boys aged 8-10 have fully retractile foreskin, but the percentage increases to 62.9 percent in boys aged 11-15.<ref name="kayaba1996" /> Imamura (1997) reported that 77 percent of boys aged 11-15 had retractile foreskin.<ref name="imamura1997" /> Thorvaldsen & Meyhoff (2005) conducted a survey of 4000 young men in [[Denmark]]. They reported that the mean age of first foreskin retraction is 10.4 years in [[Denmark]].<ref name="Thorvaldsen">{{REFjournal | + | [[Jakob Øster]], a Danish physician who conducted school examinations, reported his findings on the examination of school-boys in [[Denmark]], where [[circumcision]] is rare.<ref name="Øster1968">{{OesterJ 1968}}</ref> Øster (1968) found that the incidence of fusion of the [[foreskin]] with the [[glans penis]] steadily declines with increasing age and foreskin retractability increases with age.<ref name="Øster1968"/> Kayaba et al. (1996) also investigated the development of foreskin retraction in boys from age 0 to age 15.5 Kayaba et al. also reported increasing retractability with increasing age. Kayaba et al. reported that about only 42 percent of boys aged 8-10 have fully retractile foreskin, but the percentage increases to 62.9 percent in boys aged 11-15.<ref name="kayaba1996" /> Imamura (1997) reported that 77 percent of boys aged 11-15 had retractile foreskin.<ref name="imamura1997" /> Thorvaldsen & Meyhoff (2005) conducted a survey of 4000 young men in [[Denmark]]. They reported that the mean age of first foreskin retraction is 10.4 years in [[Denmark]].<ref name="Thorvaldsen">{{REFjournal |
|last=Thorvaldsen | |last=Thorvaldsen | ||
|init=MA | |init=MA | ||
| Line 444: | Line 444: | ||
|date=2001-02-01 | |date=2001-02-01 | ||
|accessdate=2019-10-17 | |accessdate=2019-10-17 | ||
| − | }}</ref> [[Complication| complications]],<ref name="Van Howe"/> difficult recovery, [[Circumcision scar| permanent injury to the appearance of the penis]], loss of [[Foreskin sensitivity| pleasurable erogenous sensation]],<ref>{{REFjournal | + | }}</ref> [[Complication| complications]],<ref name="Van Howe"/> difficult recovery, [[Circumcision scar| permanent injury to the appearance of the penis]], extreme loss of [[Foreskin sensitivity| pleasurable erogenous sensation]],<ref>{{REFjournal |
|last=Williams | |last=Williams | ||
|init=N | |init=N | ||
| Line 515: | Line 515: | ||
* [[Forced retraction]] | * [[Forced retraction]] | ||
* [[Foreskin Care for Boys]] | * [[Foreskin Care for Boys]] | ||
| + | * [[Foreskin sensitivity]] | ||
* [[Gliding action]] | * [[Gliding action]] | ||
* [[Penis]] | * [[Penis]] | ||
* [[Phimosis]] | * [[Phimosis]] | ||
* [[Preputioplasty]] | * [[Preputioplasty]] | ||
| + | * [[Stretching]] | ||
* [[Synechia]] | * [[Synechia]] | ||
* [[Risks and complications]] | * [[Risks and complications]] | ||
| Line 606: | Line 608: | ||
|date=2016-07 | |date=2016-07 | ||
|accessdate=2019-11-08 | |accessdate=2019-11-08 | ||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
}} | }} | ||
* {{REFweb | * {{REFweb | ||
| Line 643: | Line 630: | ||
{{REF}} | {{REF}} | ||
| + | |||
| + | [[Category:Education]] | ||
[[Category:Physiology]] | [[Category:Physiology]] | ||
[[Category:Parental information]] | [[Category:Parental information]] | ||
| + | |||
[[Category:From Intactipedia]] | [[Category:From Intactipedia]] | ||
[[Category:From IntactWiki]] | [[Category:From IntactWiki]] | ||
[[de:Zurückziehen der Vorhaut]] | [[de:Zurückziehen der Vorhaut]] | ||
Revision as of 16:18, 29 February 2024
Infant boys are born with a non-retractable foreskin. The development of retractable foreskin occurs gradually over a widely-variable number of years.
In the majority of adult men, the foreskin normally retracts to reveal the head of the penis. In newborns, it is normal for the foreskin to be fused to the head of the penis by the synechia, thus rendering it non-retractable. The preputial sac is sealed by the synechia.[1] The foreskin usually separates from the glans and becomes retractable with increasing age. There is much uncertainty among health care workers about when the foreskin of a boy should become retractable.[2] The mistaken belief that the foreskin was supposed to be retractable at the time of birth of the infant has led to a characterization of the genitalia of most infant males as defective at birth. This has led to many false diagnoses of phimosis, followed by unnecessary circumcision, when, in fact, the foreskin is developmentally normal. There is no one correct age for the foreskin to become retractable.
Normally, developmental non-retractability does not cause any problems, in fact, it is protective of the glans penis and protects against meatal stenosis. Non-retractability may be deemed pathological if it causes problems, such as difficulty urinating or performing normal sexual functions, but even then, this is rare, and, if the non-retractability itself is not caused by pathological inflammation, it cannot be called "pathological" or "true phimosis." A foreskin that is so narrow it will retract very little or not at all, but is not the result of a pathological inflammation, is accurately termed preputial stenosis (narrow prepuce), and will respond to treatment including steroid creams, manual stretching, and changing masturbation habits.
Contents
History
The first data on development of retractile foreskin were provided in 1949 by the famous British paediatrician, Douglas Gairdner.[3] His data have been incorporated into many textbooks and is still being repeated in the medical literature today. Gairdner said that 80 percent of boys should have a retractable foreskin by the age of two years, and 90 percent of boys should have a retractable prepuce by the age of three years.[3]
Unfortunately, Gairdner’s data are inaccurate,[4] [5] [6] so most healthcare providers have been taught inaccurate data.[5] Retractability usually occurs much later than previously believed.[4] This page provides accurate data, derived from newer and better studies, for healthcare providers.
Current view
Almost all boys are born with the inner foreskin mucosa fused with the underlying glans penis by the synechia. Most also have a narrow foreskin that cannot retract. Non-retractile foreskin is normal at birth and remains in the normal range until after puberty (age 18). The non-retractile foreskin is nature's way of protecting the young boy from meatal stenosis and infection in the preputial sac.
Some boys develop retractile foreskin earlier, and about 2 percent of males have a non-retractile foreskin throughout life. Non-retractile foreskin is not a disease and does not require treatment.
There are three possible conditions that cause non-retractile foreskin:
- Tightness of the foreskin orifice
- Fusion of the foreskin with the glans penis[7]
- Frenulum breve (which is rare and cannot be diagnosed until the previous two reasons have been eliminated).
The first two reasons are normal in childhood and are not pathological in children. The third can be treated conservatively, retaining the foreskin.
Infants and pre-school
Kayaba et al. (1996) reported that before six months of age, no boy had a retractable prepuce; 16.5 percent of boys aged 3-4 had a fully retractable prepuce.[8] Imamura (1997) examined 4521 infants and young boys. He reported that the foreskin is retractile in 3 percent of infants aged one to three months, 19.9 percent of those aged ten to twelve months, and 38.4 percent of three-year-old boys.[9] Ishikawa & Kawakita (2004) reported no retractability at age one, (but increasing to 77 percent at age 11-15).[10] Ko et al. (2007) examined 59 newborn Taiwanese boys. Not one had a retractable foreskin.[11]
Non-retractile foreskin is the normal, expected, and more usual condition in this age group.[12] Ballooning of the foreskin may occur in this age group.
School-age and adolescence
Jakob Øster, a Danish physician who conducted school examinations, reported his findings on the examination of school-boys in Denmark, where circumcision is rare.[13] Øster (1968) found that the incidence of fusion of the foreskin with the glans penis steadily declines with increasing age and foreskin retractability increases with age.[13] Kayaba et al. (1996) also investigated the development of foreskin retraction in boys from age 0 to age 15.5 Kayaba et al. also reported increasing retractability with increasing age. Kayaba et al. reported that about only 42 percent of boys aged 8-10 have fully retractile foreskin, but the percentage increases to 62.9 percent in boys aged 11-15.[8] Imamura (1997) reported that 77 percent of boys aged 11-15 had retractile foreskin.[9] Thorvaldsen & Meyhoff (2005) conducted a survey of 4000 young men in Denmark. They reported that the mean age of first foreskin retraction is 10.4 years in Denmark.[14] Non-retractile foreskin is the more common condition until about 10-11 years of age.
Ko et al. (2007) examined 1145 Taiwanese boys aged 7 to 13. Ko et al. reported:
Our findings indicate that the degree of preputial retractability increases with age, while the prevalence of unretractable prepuce decreases with age. By the age of 13 years, very few boys (some 0.3%) still had an unretractable prepuce (i.e. type 1 prepuce).[11]
The findings reported by Ko et al. are consistent with the findings reported by Øster (1968), by Kayaba et al. (1996), and by Thorvaldsen & Meyhoff (2005)
Discussion
Boys usually are born with a non-retractile foreskin. The foreskin gradually becomes retractable over a variable period of time ranging from birth to 18 years or more.[13][14] There is no “right” age for the foreskin to become retractable. Non-retractile foreskin does not threaten health so no intervention is necessary. Many boys only develop a retractable foreskin after puberty. Education of concerned parents usually is the only action required.[15]
Avoidance of premature retraction
Care-givers and healthcare providers must be careful to avoid premature retraction of the foreskin, which is contrary to medical recommendations, painful, traumatic, tears the attachment points (synechiae), may cause infection, is likely to generate medico-legal issues, and may cause paraphimosis, with the tight foreskin acting like a tourniquet. The first person to retract the boy’s foreskin should be the boy himself.[4] [16]
Making the foreskin retractable
Teen boys who still have a non-retractable foreskin (about 10 percent of boys) should start stretching exercises to make the foreskin retractable in preparation for adult life.
Occasionally a male reaches adulthood with a non-retractile foreskin. Some men with a non-retractile foreskin happily go through life and father children. Other men, however, may want to make their foreskin retractile.
Fixing a narrow foreskin
The foreskin can be made retractable by:
- Manual stretching[17][18]
- Application of topical steroid ointment to assist the stretching.[19][20]
See Phimosis for more information.
Fixing a fused foreskin
In a few cases, the synechial fusion of childhood lingers past puberty. After puberty, the synechial fusion should be about ready to spontaneously release the foreskin from the glans penis. One may try gently peeling the foreskin away from the glans penis by using one's thumbs. It may take one several tries to get it all separated. Do not force anything and do not cause cause yourself pain.
Apply petroleum jelly after separation occurs for about two weeks to prevent re-adhesion.
If one is unsuccessful, then one may need to consult a urologist.
Issues with circumcision as treatment
Male circumcision is outmoded as a treatment for non-retractile foreskin, but it is still recommended by many urologists because of lack of adequate information, and perhaps because of the profit to the doctor associated with circumcision. Nevertheless, circumcision should be avoided whenever possible because of pain, trauma, cost,[21][22] complications,[21] difficult recovery, permanent injury to the appearance of the penis, extreme loss of pleasurable erogenous sensation,[23] impairment of erectile and ejaculatory functions,[24][25] and adverse sexual and psychological effects.
Adult foreskin
Should the foreskin retract automatically when the penis becomes erect?
The answer to this question depends on the relative length of the foreskin in relation to the length of the penis. If the foreskin is shorter than the erect penis, then it will retract automatically on erection. On the other hand, if the foreskin is longer than the erect penis, then automatic retraction will not occur. This condition is not viewed as a problem.
A very few of the longest foreskins will not stay retracted when manually retracted. Instead, they will spontaneously glide forward when released. This condition is believed to be very rare.
See Foreskin length.
See also
- Attachment of the foreskin
- Ballooning of the foreskin
- Forced retraction
- Foreskin Care for Boys
- Foreskin sensitivity
- Gliding action
- Penis
- Phimosis
- Preputioplasty
- Stretching
- Synechia
- Risks and complications
- Tissue expansion
External links
 Wallerstein, Edward: When Your Baby Boy is Not Circumcised (Four-page pamphlet), Pennypress (Seattle). (February 1982). Retrieved 14 May 2021.
Wallerstein, Edward: When Your Baby Boy is Not Circumcised (Four-page pamphlet), Pennypress (Seattle). (February 1982). Retrieved 14 May 2021. Milos, Marilyn (September 2007).
Milos, Marilyn (September 2007). Answers to Your Questions About Premature (Forcible) Retraction of Your Young Son's Foreskin
, NOCIRC. Retrieved 2 December 2019.
Quote:The first person to retract a child’s foreskin should be the child himself.
 Sorrells, Morrie (2008).
Sorrells, Morrie (2008). The Development of Retractile Foreskin in the Child and Adolescent
 , Doctors Opposing Circumcision (D.O.C.). Retrieved 13 August 2020.
, Doctors Opposing Circumcision (D.O.C.). Retrieved 13 August 2020.
Quote:Male circumcision is an outmoded treatment for non-retractile foreskin, but it is still recommended by many urologists because of lack of adequate information and understanding of alternative methods of relief. Nevertheless, circumcision should be avoided because of pain, trauma, cost, complications, difficult recovery, permanent injury to the appearance of the penis, loss of pleasurable erogenous sensation, and impairment of erectile and ejaculatory functions.
 (14 November 2008).
(14 November 2008). Normal development of the prepuce: Birth through age 18
, Circumcision Information Reference Library. Retrieved 8 November 2019. Helard, Lou (1 August 2014).
Helard, Lou (1 August 2014). Functions of the Foreskin
, Intact Australia. Retrieved 29 May 2020. Care of the Intact (Not Circumcised) Penis in the Young Child
Care of the Intact (Not Circumcised) Penis in the Young Child  , Doctors Opposing Circumcision (D.O.C.). (July 2016). Retrieved 8 November 2019.
, Doctors Opposing Circumcision (D.O.C.). (July 2016). Retrieved 8 November 2019. (July 2018).
(July 2018). The penis and foreskin
, www.rch.org.au, Royal Children's Hospital of Melbourne. Retrieved 6 July 2020.
- NSFW How the foreskin works
References
- ↑
 Taylor JR, Lockwood AP, Taylor AJ. The prepuce: specialized mucosa of the penis and its loss to circumcision. Br J Urol. 1996; 77: 291-5. PMID. DOI. Retrieved 23 September 2019.
Taylor JR, Lockwood AP, Taylor AJ. The prepuce: specialized mucosa of the penis and its loss to circumcision. Br J Urol. 1996; 77: 291-5. PMID. DOI. Retrieved 23 September 2019.
- ↑
 Simpson ET, Barraclough P. The management of the paediatric foreskin. Aust Fam Physician. May 1998; 27(4): 381-383. PMID. Retrieved 17 October 2019.
Simpson ET, Barraclough P. The management of the paediatric foreskin. Aust Fam Physician. May 1998; 27(4): 381-383. PMID. Retrieved 17 October 2019.
- ↑ a b
 Gairdner DMT. The fate of the foreskin: a study of circumcision. British Medical Journal. 1949; 2(4642): 1433-7. PMID. PMC. DOI. Retrieved 28 October 2019.
Gairdner DMT. The fate of the foreskin: a study of circumcision. British Medical Journal. 1949; 2(4642): 1433-7. PMID. PMC. DOI. Retrieved 28 October 2019.
- ↑ a b c
 Wright JE. Further to the "Further Fate of the Foreskin". Med J Aust. 7 February 1994; 160: 134-135. PMID. Retrieved 17 October 2019.
Wright JE. Further to the "Further Fate of the Foreskin". Med J Aust. 7 February 1994; 160: 134-135. PMID. Retrieved 17 October 2019.
- ↑ a b
 Hill G. Circumcision for phimosis and other medical indications in Western Australian boys. Med J Aust. 2 June 2003; 178(11): 587. PMID. Retrieved 17 October 2019.
Hill G. Circumcision for phimosis and other medical indications in Western Australian boys. Med J Aust. 2 June 2003; 178(11): 587. PMID. Retrieved 17 October 2019.
- ↑
 Denniston GC, Hill G. Gairdner was wrong. Can Fam Physician. 1 October 2010; 56(10): 986-7. PMID. PMC. Retrieved 17 October 2019.
Denniston GC, Hill G. Gairdner was wrong. Can Fam Physician. 1 October 2010; 56(10): 986-7. PMID. PMC. Retrieved 17 October 2019.
- ↑
 Deibart GA. The separation of the prepuce in the human penis. Anat Rec. 1933; 57: 387-99. DOI. Retrieved 7 October 2019.
Deibart GA. The separation of the prepuce in the human penis. Anat Rec. 1933; 57: 387-99. DOI. Retrieved 7 October 2019.
- ↑ a b
 Kayaba H, Tamura H, Kitajima S, et al. Analysis of shape and retractability of the prepuce in 603 Japanese boys. J Urol. 1 November 1996; 156(5): 1813-1815. PMID. Retrieved 19 October 2019.
Kayaba H, Tamura H, Kitajima S, et al. Analysis of shape and retractability of the prepuce in 603 Japanese boys. J Urol. 1 November 1996; 156(5): 1813-1815. PMID. Retrieved 19 October 2019.
- ↑ a b
 Imamura E. Phimosis of infants and young children in Japan. Acta Paediatr Jpn. 1997; 39(3): 403-405. PMID.
Imamura E. Phimosis of infants and young children in Japan. Acta Paediatr Jpn. 1997; 39(3): 403-405. PMID.
- ↑
 Ishikawa E, Kawakita M. Preputial development in Japanese boys. Hinyokika Kiyo. 2004; 50(5): 305-308. Retrieved 8 November 2019.
Ishikawa E, Kawakita M. Preputial development in Japanese boys. Hinyokika Kiyo. 2004; 50(5): 305-308. Retrieved 8 November 2019.
- ↑ a b
 Ko MC, Liu CK, Lee WK, Jeng HS, Chiang HS, Li CY. Age-specific Prevalence Rates of Phimosis and Circumcision in Taiwanese Boys. Journal of the Formosan Medical Association. April 2007; 106(4): 302-7. PMID. DOI. Retrieved 8 November 2019.
Ko MC, Liu CK, Lee WK, Jeng HS, Chiang HS, Li CY. Age-specific Prevalence Rates of Phimosis and Circumcision in Taiwanese Boys. Journal of the Formosan Medical Association. April 2007; 106(4): 302-7. PMID. DOI. Retrieved 8 November 2019.
- ↑
 Agawal A, Mohta A, Anand RK. Preputial retraction in children. Journal of Indian Association of Pediatric Surgeons. 2005; 10(2): 89-91. DOI. Retrieved 9 December 2019.
Agawal A, Mohta A, Anand RK. Preputial retraction in children. Journal of Indian Association of Pediatric Surgeons. 2005; 10(2): 89-91. DOI. Retrieved 9 December 2019.
- ↑ a b c
 Øster J. Further Fate of the Foreskin: Incidence of Preputial Adhesions, Phimosis, and Smegma among Danish Schoolboys
Øster J. Further Fate of the Foreskin: Incidence of Preputial Adhesions, Phimosis, and Smegma among Danish Schoolboys  . Arch Dis Child. 1968; 43(228): 200-3. PMID. PMC. DOI. Retrieved 18 June 2024.
. Arch Dis Child. 1968; 43(228): 200-3. PMID. PMC. DOI. Retrieved 18 June 2024.
- ↑ a b
 Thorvaldsen MA, Meyhoff H. Patologisk eller fysiologisk fimose? [Pathological or physiological phimosis?] (Danish). Ugeskr Læger. 2005; 167(17): 1858-1862. Retrieved 17 October 2019.
Thorvaldsen MA, Meyhoff H. Patologisk eller fysiologisk fimose? [Pathological or physiological phimosis?] (Danish). Ugeskr Læger. 2005; 167(17): 1858-1862. Retrieved 17 October 2019.
- ↑
 Spilsbury K, Semmens JB, Wisniewski ZS, et al. Circumcision for phimosis and other medical indications in Western Australian boys. Med J Aust. 17 February 2003; 178(4): 155-158. PMID. Retrieved 17 October 2019.
Spilsbury K, Semmens JB, Wisniewski ZS, et al. Circumcision for phimosis and other medical indications in Western Australian boys. Med J Aust. 17 February 2003; 178(4): 155-158. PMID. Retrieved 17 October 2019.
- ↑
 (2019).
(2019). Doctors Opposing Forcible Retraction
, Doctors Opposing Forcible retraction. Retrieved 2 October 2019. - ↑
 Dunn HP. Non-surgical management of phimosis. Aust N Z J Surg. 1989; 59(12): 963. PMID. DOI.
Dunn HP. Non-surgical management of phimosis. Aust N Z J Surg. 1989; 59(12): 963. PMID. DOI.
- ↑
 Beaugé M. The causes of adolescent phimosis. Br J Sex Med. 1997; (Sept/Oct): 26. Retrieved 18 October 2019.
Beaugé M. The causes of adolescent phimosis. Br J Sex Med. 1997; (Sept/Oct): 26. Retrieved 18 October 2019.
- ↑
 Orsola A, Caffaratti J, Garat JM. Conservative treatment of phimosis in children using a topical steroid. Urology. 2000; 56(2): 307-310. PMID. DOI. Retrieved 18 October 2019.
Orsola A, Caffaratti J, Garat JM. Conservative treatment of phimosis in children using a topical steroid. Urology. 2000; 56(2): 307-310. PMID. DOI. Retrieved 18 October 2019.
- ↑
 Ashfield JE, Nickel KR, Siemens DR, et al. Treatment of phimosis with topical steroids in 194 children. J Urol. March 2003; 169(3): 1106-1108. PMID. DOI. Retrieved 18 October 2019.
Ashfield JE, Nickel KR, Siemens DR, et al. Treatment of phimosis with topical steroids in 194 children. J Urol. March 2003; 169(3): 1106-1108. PMID. DOI. Retrieved 18 October 2019.
- ↑ a b
 Van Howe RS. Cost-effective treatment of phimosis. Pediatrics. October 1998; 102(4): e43. PMID. Retrieved 17 October 2019.
Van Howe RS. Cost-effective treatment of phimosis. Pediatrics. October 1998; 102(4): e43. PMID. Retrieved 17 October 2019.
- ↑
 Berdeu D, Sauze L, Ha-Vinh P, Blum-Boisgard C. Cost-effectiveness analysis of treatments for phimosis: a comparison of surgical and medicinal approaches and their economic effect.. BJU Int. 1 February 2001; 87(3): 239-244. PMID. DOI. Retrieved 17 October 2019.
Berdeu D, Sauze L, Ha-Vinh P, Blum-Boisgard C. Cost-effectiveness analysis of treatments for phimosis: a comparison of surgical and medicinal approaches and their economic effect.. BJU Int. 1 February 2001; 87(3): 239-244. PMID. DOI. Retrieved 17 October 2019.
- ↑
 Williams N, Kapila L. Complications of circumcision. Brit J Surg. 1993; 80: 1231-1236. PMID. DOI. Retrieved 17 October 2019.
Williams N, Kapila L. Complications of circumcision. Brit J Surg. 1993; 80: 1231-1236. PMID. DOI. Retrieved 17 October 2019.
- ↑
 Shen Z, Chen S, Zhu C, et al. Erectile function evaluation after adult circumcision. Zhonghua Nan Ke Xue. 1 January 2004; 10(1): 18-19. PMID. Retrieved 17 October 2019.
Shen Z, Chen S, Zhu C, et al. Erectile function evaluation after adult circumcision. Zhonghua Nan Ke Xue. 1 January 2004; 10(1): 18-19. PMID. Retrieved 17 October 2019.
- ↑
 Masood S, Patel HRH, Himpson RC, et al. Penile sensitivity and sexual satisfaction after circumcision: Are we informing men correctly?. Urol Int. 2005; 75(1): 62-65. PMID. DOI. Retrieved 17 October 2019.
Masood S, Patel HRH, Himpson RC, et al. Penile sensitivity and sexual satisfaction after circumcision: Are we informing men correctly?. Urol Int. 2005; 75(1): 62-65. PMID. DOI. Retrieved 17 October 2019.
- ↑