Circumcision
"Male circumcision (from Latin circumcidere, meaning "to cut around") is the surgical removal or amputation of the foreskin (prepuce) part of the human penis. The foreskin comprises more than fifty percent of the epithelium of the penis.[1] When the "cutting around" is performed, the foreskin falls off, so amputation and mutilation is the result. The amputation destroys the many protective, immunological, sexual, and sensory physiological functions of the foreskin, so it is a very harmful and painful surgery.
Cepeda-Emiliani et al. (2023) commented:
Taking the sleve technique as an example of surgical flexibility during circumcision, to the extent that this technique is of such versatility that it allows highly variable quantities of cutaneous and subcutaneous tissue to be excised directly from the penile body, and to the extent that the prepuce is still conceived by segments of the medical community as "just a small piece of skin", we are concerned that aggressive circumcisions are intentionally or unintentionally being performed in pediatric and adult patients in the belief that "redundant" or " extra" tissue is being excised, or in the belief that "excesive sensitivity" is being reduced to augment ejaculatory latency time.[2]
The un-anesthetized and un-sedated newborn infant is restrained by being strapped to a special plastic board called the circumstraint. The procedure is most often an elective, non-therapeutic surgery without medical indication performed on neonates and children for religious and cultural reasons in violation of the child's human rights to physical integrity, but in older patients may be rarely indicated for therapeutic reasons. It is a radical treatment option for pathological phimosis, refractory balanoposthitis and chronic urinary tract infections (UTIs); it is contraindicated in cases of certain genital structure abnormalities or poor general health.
Posthectomy is a more accurate medical term that more accurately reflects the injury and loss of functional body tissue, but the Biblical euphemism, circumcision, is more commonly used.
With reference to involuntary, non-therapeutic circumcision of children, Child Genital Cutting (CGC) is a newer term that has been introduced to avoid issues associated with more traditional terms. Bollinger (2023) identifed CGC as an adverse childhood experience.[3]
Deacon & Muir (2022) have reviewed the evidence and concluded that "there is no medical justification for performing a circumcision prior to an age that he can assess the known risks and potential benefits, and choose to give or withhold informed consent himself."[4]
The practice of non-therapeutic circumcision of boys has greatly declined in Australia, Canada, New Zealand and the United Kingdom. It has been gradually declining since 1985 in the United States.
Contents
- 1 Historical background
- 2 Rationale
- 3 Non-medical indications for circumcision
- 4 Circumcision methods
- 5 Pain
- 6 Risks and effects
- 7 Complications
- 8 Forced circumcision
- 9 Video
- 10 Recommendations of medical authorities
- 11 British family court opinion
- 12 Rights and ethics
- 13 See also
- 14 External links
- 15 References
Historical background
The amputation of the foreskin is a very old ritual, whose exact origin cannot be verified beyond doubt. Circumcision is believed to have originated in east Africa near the Red Sea well before the dawn of recorded history.[5] Medical historians assume that circumcision already served in ancient history as a way to control the sexuality of slaves and members of the lower classes without compromising their ability to reproduce. In religious history circumcision may be seen as a substitute for human sacrifice. In prehistoric times it was not uncommon to placate the gods with human sacrifice. Castration of slaves or conquered enemies was common as well. Following religious changes this sacrifice was altered, and only a part of the very organ responsible for the creation of new life was sacrificed.
For the Aborigines, the Australian natives, the tradition of circumcision is said to go back to 10,000 BC. On the African continent, the first circumcisions are assumed to have emerged around 6000 BC. From ancient Egypt hints of various forms of circumcision date back to the time around 3000-2000 BC. The oldest known depiction[6] is an Egyptian tomb relief from the 6th dynasty, approximately 2300-2000 BC. It is not known precisely who was circumcised and why in those times.
In many cultures circumcision during puberty serves as a rite of passage, bringing adolescents into the community. As with other painful or humiliating initiation rites, proof of courage and mastering of critical situations are the key motivations. From some African tribes it is also known that the amputation of the foreskin is seen as the removal of an inborn piece of femininity from the boys, thus making them men.
Judaism
In Judaism, the tradition of circumcision goes back to the Abrahamic covenant in a passage in the Book of Genesis (17:10-14). It is seen as a covenant between God and man, dating back to the patriarch Abraham. The validity of this passage is increasingly being questioned.
| “ | 10 This is my covenant with you and your descendants after you, the covenant you are to keep: Every male among you shall be circumcised. 11 You are to undergo circumcision, and it will be the sign of the covenant between me and you. 12 For the generations to come every male among you who is eight days old must be circumcised, including those born in your household or bought with money from a foreigner—those who are not your offspring. 13 Whether born in your household or bought with your money, they must be circumcised. My covenant in your flesh is to be an everlasting covenant. 14 Any uncircumcised male, who has not been circumcised in the flesh, will be cut off from his people; he has broken my covenant.” – Bible (Gen 17, 10-14, NIV) |
According to the anthropologist and sociologist Rabbi Nissan Rubin, the Jewish form of circumcision, called brit mila, during the first two millennia did not include the later customary periah, namely the complete scraping of the inner foreskin from the glans. This was only added around 135 AD, to make it almost impossible to restore the foreskin by stretching, which became popular in the wake of Hellenic influence. While originally only the tip of the foreskin was cut off, periah removes the entire foreskin.
In the Greek society of the day, a denuded glans was considered obscene and risible. In ultra-orthodox communities, circumcision is followed by the mohel, the ritual circumciser, sucking blood from the wound with his mouth. This practice is highly controversial, as it can result in an infection with herpes simplex type 1. In New York City, between 2000 and 2011 eleven children were infected with herpes, 10 of whom had to be treated in hospital. Two of them suffered permanent brain damage, two others died. In the 12th century, the Jewish philosopher and doctor Maimonides claimed that circumcision was necessary, as it diminished sexual desires and reduced the pleasure to a degree just sufficient for mere reproduction.
Christianity
Jesus was born into a Jewish family in Israel, where Judaism was the prevailing religion, so He was circumcised on the eighth day.[7]
The first Christians had been born Jewish, so a question arose whether one must be circumcised to be a Christian. When Christian leaders met at the Council at Jerusalem in the First Century to decide what was required to be a Christian, a letter was written to explain the requirements, but circumcision was omitted from the requirements.[8]
In Christianity, circumcision is practiced only in Coptic churches. There is no general belief that circumcision is a requirement of Christianity.[9]
Nevertheless, Christian moral notions had decisive influence on the spread of this practice. In the puritan influenced USA, circumcision of children was popular in the 19th century as a means to prevent masturbation. In those days, this so-called ‘self-abuse‘ was not only considered immoral, but was supposedly responsible for a variety of diseases. Masturbation, however, is not mentioned anywhere in the Holy Bible, so there is no support for the belief that it is somehow immoral or sinful.
Even the mere existence of a foreskin was linked to many illnesses. Among them one could find syphilis, epilepsy, paralysis of the spine, bed wetting, scoliosis (spinal deformity), paralysis of the bladder, club foot, nerve pain in the lower abdomen, tuberculosis and lazy eye. One of the best known advocates of child circumcision was John Harvey Kellogg, co-inventor of the corn flakes bearing his name. In 1888, he wrote:
| “ | A remedy which is almost always successful in small boys is circumcision, especially when there is any degree of phimosis. The operation should be performed by a surgeon without administering an anaesthetic, as the brief pain attending the operation will have a salutary effect upon the mind, especially if it be connected with the idea of punishment, as it may well be in some cases. In females, the author has found the application of pure carbolic acid to the clitoris an excellent means of allaying the abnormal excitement, and preventing the recurrence of the practice in those whose will-power has become so weakened that the patient is unable to exercise entire self-control. – John Harvey Kellogg[10] |
Islam
In Islam, circumcision is also religiously founded, even though there is no mention of it in the Koran itself. According to tradition, the Prophet Mohammed was born without a foreskin. It is seen as a sign of prophets that they are born without a foreskin already. It is considered an honour to "resemble the example of the Prophet", meaning to be circumcised. In Islam, unlike Judaism, there is no specific age at which the circumcision should be performed. Most circumcisions take place at ages between 6 and 10 years, but the range goes from birth to adulthood.
Rationale
Reasons for performing circumcision range widely by culture, religion, location, and age.
Cultural
Many cultures perform circumcision as a rite of passage into manhood. This is common in the Middle East and amongst some indigenous African and Southeast Asian peoples.
The United States and Israel are the only industrialized countries in the world to have a high incidence of non-therapeutic infant male circumcision. The vast majority of infant circumcisions performed in the United States are for non-religious, non-medical reasons. See History of circumcision.
Religious
The circumcision of newborn boys is seen as a divine commandment in the Jewish faith. Though absent in the Koran, male circumcision is considered a religious requirement in Islam, and it is performed on male children of varying ages. Converts to these faiths may also choose to undergo circumcision, but it is not always required.
Medical indication
There are no medical indications for circumcision of the newborn. The circumcision industry offers circumcision of the newborn to the public because of the financial incentive.
The form of circumcision adopted by the medical community essentially was equivalent to the Jewish form with periah, so it inflicted the maximum injury.
In a few cases with older patients, circumcision is legitimately indicated; a patient may be suffering recurring infections, and other methods of treatment have failed. In other cases, a patient may be suffering from a severe case of phimosis. Overall, the actual medical necessity for circumcision is extremely rare since many conditions respond to conservative treatment. All circumcisions injure the patient by amputating the foreskin its with many protective, immunological, sensory, and sexual functions.
- Deformed or malformed foreskin. A foreskin so deformed or malformed that it does not function properly may be removed by circumcision.
- Traumatically injured foreskin. A foreskin so traumatically damaged foreskin that cannot be surgically repaired is a valid medical reason for circumcision.
- Diseased foreskin. A foreskin that is diseased is a valid indication for cirumcision. Some diseases that qualify are malignancy, lichen sclerosis, yeast infection in men with diabetes, and recurrent balanoposthitis.
In such cases, the benefit of removing the problem foreskin may exceed the maleficial harms of tissue and function destruction.
Arguments of prophylaxia
Though the practice of ritual circumcision of males, both consenting and non-consenting, has existed for millenia, the search for "potential medical benefits" began relatively recently. {Potential means to exist in possibility, but not in actuality, so a "potential benefit" is not a genuine proven benefit.) The discussion of circumcision in the Ninth Edition of the Encyclopǽdia Britannica (1876) made no mention of any prophylactic, medical, or therapeutic value or function.[11]
Initially, circumcision was adopted in the 19th century as a way to stop boys and men from masturbating, when masturbation was claimed to be the cause for many diseases. As the myth that circumcision prevented masturbation became debunked, advocates of circumcision began the great search to find the "medical benefits" of circumcision.
Male and female circumcision involves the removal and disruption of normal anatomical structures that are primary areas of sexual sensation.[1] In the past, some advocates of mass circumcision have considered the prepuce to be a "mistake of nature," but this notion has no validity because the prepuce is ubiquitous in primates and because it provides functional advantages.[12]
All claims that circumcision prevents future disease are false.[13] They are made to enable a physician to perform circumcision and collect a fee.
Search for prophylactic reasons
The practice of finding prophylactic reasons for infant circumcision started in Germany in the nineteenth century, when non-Jewish Germans criticized the Jewish practice of infant circumcision as being barbaric, Jewish doctors sprang to the defense of the religious practice by claiming health benefits.[14] And so started the long tradition of Jewish doctors inventing reasons for circumcision (and deceving gentile doctors).
Following the discovery of bacteria as a cause of many diseases – such as tuberculosis – the search began for other illnesses that could be prevented by circumcision.
In 1870 the prominent Dr. Lewis A. Sayre of NYC’s famed Bellevue Hospital[15] claimed to cure a boy’s paralyzed legs with circumcision. Sayre's wild advocacy of circumcision exemplified how some circumcision facts and myths originated. He also claimed to cure epilepsy, mental disorders, hip-joint pain, & hernias with circumcision. “Genital irritations” & masturbation were deemed to be the cause of these issues. Sayre was later elected as the President of the American Medical Association. [16]
In the 1920s it was penile cancer. Abraham L. Wolbarst (1926) claims that circumcision can prevent penile cancer.[17]
In the 1940s, prostate and tongue cancer as well as STDs. Eugene H. Hand (1949) falsely explains that circumcision somehow protects against venereal diseases and tongue cancer.[18]
In the 1950s it was cervical cancer. Abraham Ravich (1951) invents the myth that circumcision reduces the risk of women getting cervical cancer.[19]
In the late 1960s it was neuroses. Morris Fishbein (1969) calls for circumcision to prevent nervousness and, of course, masturbation.[20]
In the 1970s bladder- and rectal cancer. Abraham Ravich (1971) claims that circumcision would prevent bladder cancer and rectal cancer.[21]
In the 1980s, UTIs. Thomas E. Wiswell (1985) claims that circumcision, using a methodologically flawed report, reduces the risk of urinary tract infections.[22]
Aaron J. Fink (1986), with no evidence whatsoever, claims that circumcision protects against AIDS followed.[23]
Retrospectively, circumcision was always advertised as a cure for whatever disease was in the public spotlight at the time. Doctors Opposing Circumcision (D.O.C.) (2016) state:
These claims date originally from before the advent of evidence-based medicine, when doctors relied on the opinions of other clinicians to inform their practice, rather than on scientifically collected evidence.[24]
The sheer mass of studies and publications that were released during those almost 180 years on this topic are the reason that even arguments that have been disproved multiple times, especially regarding infant and child circumcision, tenaciously persist up until today.
An ever-recurring element of initiation rites found in many different cultures is the fixation upon the genitalia.
It reflects the fascination that emerges from the ability to create new life. In most cultures, fertility is seen as the most precious good, and the body parts involved frequently find themselves in the focus of ritual acts. In many parts of the world, those rites take place when the boy reaches puberty, and are meant to symbolize his transition from boy to man. The removal of the male foreskin is just one of many phenomena that developed in this context. They range from the removal of the frenulum in boys and men through partial or complete removal of the foreskin up to radical operations. Australian Aborigines, as mentioned above, have their foreskins removed. It is also usual that, a few weeks later, young men have their penises sliced open in a subincision, resulting in a partly or completely divided urethra.
Another known, particularly massive, intervention is the stripping of the entire skin off the penis. In Indonesia, boys have metal or bamboo balls inserted into their penis shaft or glans at the beginning of puberty, which form little "humps".
For many cultures it is also common to perform similar rituals on girls. This can range from relatively small interventions such as piercing or cutting the clitoral hood, to its complete removal and up to radical removal of clitoral hood, clitoris, inner and outer labia followed by sewing up the vagina.
The following text is taken from the Circumpendium.
Prophylactic reasons
Some people claim that circumcision has prophylactic benefits. Especially in the USA those arguments have persisted for more then a 100 years, with ever changing diseases circumcision is said to protect against. At first, these were diseases where masturbation was believed to be the cause. After bacteria and viruses had been discovered, arguments changed, and one after another miscellaneous diseases were cited.
- Phimosis: as mentioned earlier, true phimosis is rare and can be treated effectively without surgery. According to a study by Blalock et al. (2003)[25], 2.9% of those circumcised develop a post-operative phimosis, in which the circumcision scar constricts. In intact patients, the rate of phimosis is only 1% (see also the study by Jakob Øster). Therefore, circumcision is not a preventive measure for phimosis.
- Sexually Transmitted Diseases (STDs): a vast number of studies has been conducted on the subject of transmission of STDs.
- First, it has to be noted that any form of protection against these diseases only affects people who are sexually active. Circumcision in childhood cannot be justified on these grounds, since any assumed protective effect will not occur before the boy is already old enough to decide about circumcision for himself.
- As mentioned above, the foreskin keeps the glans moist. This subpreputial moisture contains, among other substances, the enzyme lysozyme, which breaks up the cell wall of bacteria, thereby providing a natural antibacterial screen. This explains the results of several studies, such as Laumann et al.[26], which found a higher rate of infection with bacterial venereal diseases in circumcised than in intact men.
- The studies by Fleiss et al. (1998) support this.[27] According to the AAP, the general sexual behaviour of the male - such as frequent change in partners and the use of condoms - has a much higher impact on sexually transmitted diseases then the circumcision status.[28]
- HIV / AIDS: in the recent past, the argument that circumcision could help to contain the spread of HIV has been stated numerous times.
- First, two notes: for one, the use of condoms is still by far the most effective protection against an infection. During intercourse with that preventive measure, circumcision status does not make a difference.
- Secondly, the assumed protection would only affect healthy men who have intercourse with an infected woman. An infected man can infect a women by transmission of his bodily fluids, so that his circumcision status is irrelevant. Therefore, the use of condoms remains vital in containing the spread of HIV, which in return renders circumcision unnecessary
- Due to the inevitable loss of sensitivity as a result of circumcision, there is also the temptation to go without condoms, in order not to lose even more sensitivity.[29][30][31]
- Two studies that have been published in early 2007[32][33], which investigated the effectiveness of circumcision as a means of reducing the spread of HIV from infected women to heterosexual men in African high risk areas, have been repeatedly subjected to strong criticism. Both studies were ended prematurely, which distorted the results. The men who had been circumcised for the study had to stay sexually inactive during the wound healing, which gave the intact control group more relative opportunity to become infected. These African randomized clinical trials have been demonstrated to have very serious methodological and statistical errors that distort the results in favor of circumcision.[34]
The fact that the USA has both the highest rate of circumcised males in the western world, as well as the highest HIV infection rate, makes the studies look dubious. Besides that, several other studies concluded that circumcision does not have a significant impact on the risk of infection with HIV.[35][36][37][38][39]
- Urinary tract infections (UTI): a UTI can be effectively treated with antibiotics, this was also proven by studies.[40][41] A Swedish study[42] found that, during the first 6 years of life, the incidence of UTIs in boys was 1.8%, but in girls was 6.6%. UTIs are less common in boys after the first year of life. Mueller et al. [43] did not find a significant difference in UTI rates between circumcised and intact boys with normal urinary tract anatomy.
- Other studies suggest that circumcision is more likely to raise than to lower the generally low risk of acquiring UTI: multiple studies from Israel showed a strong correlation between ritual circumcision on the 8th day of life and postoperative UTI.[44][45][46]
- It can be concluded that circumcision is ineffective as a preventive measure against UTIs.
- Penile and cervical cancer / HPV: first studies on those diseases and their assumed prevention by circumcision date back to 1932, a time when the cause for those illnesses was not yet fully understood.[47] Today, it is known that sexually transmitted human papillomavirus (HPV) is a major risk factor[48], as well as smoking[49]. Studies have shown that there is no significant difference in the risk of getting penile cancer between circumcised and intact men. To prevent a single case of penile cancer, it would statistically take 600 to 900 circumcisions[50]. The influence of circumcision on the infection risk of the female partner with cervical cancer has been refuted several times as well. HPV vaccination is an effective measure against carcinoma of the cervix.
In conclusion, circumcision does not provide any proven benefits in preventive medicine.
Non-medical indications for circumcision
Apart from the medical indication of pathological phimosis, there also are other reasons for circumcision.
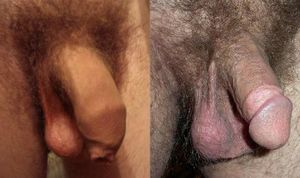
Aesthetic reasons
The visual appearance of the penis is changed radically after circumcision. In this case, personal taste is decisive whether an intact or a circumcised penis is more appealing. Since a circumcision cannot be undone, it is essential to be fully informed about the risks and possible later complications before embarking on an aesthetically motivated circumcision, to decide whether the appearance will justify such bodily modification.
It should be noted that every circumcision operation leaves a life-long circumcision scar that encircles the shaft of the penis. In addition, there frequently a a color change at the circumcision scar which results in a two-tone appearance.
Since this modification and its possible late effects will be the lifelong burden of the person who undertakes an aesthetically motivated circumcision to suit his personal preferences, a valid decision to proceed can only be made by the person to be circumcised himself, once he has reached the necessary age and level of maturity to make that decision. This should normally be the case when adulthood is reached.
Financial reasons
In the United States, payment for non-therapeutic circumcision is made by most third-party payers without question of necessity. Doctors frequently perform medically-unnecessary, non-therapeutic circumcision of infants and children simply to collect a fee for the surgical operation. The only beneficiary of such surgery is the bank account of the medical doctor.
Moral reasons
With the foreskin, circumcision removes approximately 70% of the sensitive tissue of the penis, lowering the potential for sexual stimulation accordingly. Due to the loss of around 50% of the entire penile skin, the penis loses the reserve skin that provides cutaneous mobility in the erect penis and the gliding action.
In the past, this circumstance was used to make it harder for boys to masturbate and masturbation less fun, as masturbation was viewed as immoral and was assumed to cause a variety of mental diseases, caused by the thinking of immoral thoughts! More on that can be found in the chapter "Historical background". Today, it is known that masturbation has no negative health effects, but can contribute positively to the child's sexual development. Sexuality is no longer a taboo nowadays, while masturbation is considered to be a natural part of human sexuality and is no longer seen as immoral. Therefore, circumcision for moral reasons - which would only affect boys too young to give informed consent - is no longer justifiable nowadays.
Hygiene reasons
Hygiene refers to health and only secondarily to cleanliness.
One should note that the human foreskin is endowed by nature with immunological functions that serve to protect the human body from disease.[27] The glans penis receives blood through the frenular artery.[51] These facts are generally overlooked in arguments for alleged hygienic benefits of circumcision.
A common reason stated for circumcision is the assumption of hygienic benefits. This argument has to be viewed in the context of the environment the person in question grows up in. It is commonly known that bad hygienic circumstances, especially insufficient access to clean drinking water, pose a serious problem. The situation in disaster areas or refugee camps in the so-called third world keep reminding us of that.
In western industrial nations, however, this problem does not exist, in view of the availability of clean water for daily personal hygiene. If the cleaning of the genitals is performed on a daily basis - and that may be assumed - no pathogens can accumulate under the foreskin. Cleaning of the glans and the area underneath the foreskin is easy - they are simply washed along with the rest of the body, just like the areas between the toes.
In small boys, where the foreskin cannot be retracted yet, cleaning is not necessary, since the membrane that fuses the foreskin to the glans prevents the accumulation of micro-organisms. The so-called " ballooning", where the foreskin inflates during urination, is not a serious problem.
The opening of the foreskin in small boys is often quite narrow and serves as a one-way valve, allowing the urine to flow out, but preventing entry of microbes, for example from a dirty diaper. As long as the child is able to pass water, everything works as nature intended.
But even in areas where there are poorer hygienic conditions and an insufficient access to medical care, the benefits of easier cleaning of a circumcised penis are to be viewed with a critical eye. Although even longer periods without personal hygiene will not result in an accumulation of germs under the foreskin, circumcision itself is not without risk of complications. If the operation is carried out without proper sterility, there is a high risk of an infection of the wound. This also applies to the treatment of common complications like post-operative bleeding.
The benefit of easier cleaning must be balanced against the risk of promoting serious infections - among others HIV - during the operation. In parts of Africa, several dozen of one tribe's boys die each year as a result of their circumcision.
Circumcision methods
The Circumcision methods are discussed in a separate article.
Pain
In the past, advocates of circumcision claimed that a newborn child's nerve system was not yet fully developed, and that as a result, the child felt no pain during the circumcision procedure. Anand & Hickey (1987) have shown that newborn children do in fact feel pain, and more acutely than adults.[52] This has led American health associations to recommend doctors take measures to reduce the pain of circumcision in infants.
The Circumcision Policy Statement (1999) states quite clearly that "There is considerable evidence that newborns who are circumcised without analgesia experience pain and physiologic stress". Furthermore, the pain is quite severe, and requires injections for proper pain management. Sucrose and Acetaminophen "cannot be recommended as the sole method of analgesia". Topical cream is no longer thought sufficient as "the analgesic effect is limited during the phases associated with extensive tissue trauma such as...tightening of the clamp".[53]
The AAFP (2002) states quite simply in their position paper, "Newborns experience pain during circumcision".[54] This is not a debatable fact, and yet, it is not widely accepted, even by some doctors. It might be hard for some doctors to accept, as they may have been taught that the infant does not feel pain, and may have performed countless circumcisions with this idea. Usage of anesthesia for infant circumcision is still by no means the rule.
Penile injections of anesthetic are now recommended by all of the major medical institutions. In their Report 10 of the Council on Scientific Affairs, the AMA states "When the decision is made to proceed with circumcision, local anesthesia should be provided for the procedure. Ring block or dorsal penile blocks [injections] are most effective. EMLA cream has limited utility". Alarmingly, "Despite the clear evidence that newborn males generate brisk pain responses during circumcision, a recent survey of residency training programs found that 26% of programs that taught circumcision provided no instruction on the use of local anesthesia". The AMA reports that "Of physicians performing circumcision, 45% use anesthesia, 71% of pediatricians, 56% of family practitioners, and 25% of obstetricians".[55]
The AAP's Heatlhy Children website suggests "Your pediatrician (or your obstetrician) should discuss the forms of analgesia that are available".[56] Be that as it may, few forms of analgesia are recommended. There are basically two types of injections to choose from, and the website does not go into the difference between a 'dorsal nerve block' and a 'ring block' injection.
Given what is known from aforementioned official documents, the AAP website may be more informative and effective if it would say "Make sure your doctor knows of the ineffectiveness of anything short of local anesthesia, and make sure your baby is given an injection. This is your responsibility, because your doctor may or may not be up to date on the latest understandings of infant sensitivity to pain during circumcision." The AAP may be holding back, however, perhaps because this would upset the doctor/parent power relationship, and may cause too much questioning of doctors in general. One may not expect to find this kind of advice on such a website, and yet, anything less than this is a dangerously weak statement.
To control pain, some physicians that circumcise use Tylenol, sugar,[57][58] a topical cream,[59] and/or a local anaesthetic injection called a dorsal penile ring block.[60] Topical anaesthetic only serves to numb the area to lessen the pain of the injection, but studies have shown that a dorsal penile ring block is not always effective in stopping the pain of circumcision.[61][62] During circumcision, somp physicians give children sugar pacifiers to "reduce the perception of pain",[63] but in at least one study, data shows that giving sugar to a child doesn't help to reduce the perception of pain in the child.[64] Post-operative pain and the pain the child must endure during recovery is hardly, if ever, addressed by professionals.
It has been shown that an infant's response to pain can be altered for years as a consequence of circumcision.[65][66]
Risks and effects
Just like tonsil or appendix surgery, circumcision is a surgical intervention and brings the usual risks related to surgical operations, alongside several specific risks of complications and late effects. Uberoi et al. (2022) report "some men are experiencing a complex negative constellation of psychological, physical, and sexual associations that lead to significant emotional distress directed both internally and externally. The posts also reveal a discovery phenomenon wherein men discover the physical and psychological manifestations of the decisions made by others to modify their genitals."[67]
Possible operative and postoperative complications
Circumcision is surgery. Surgical complications of circumcision generally may be classified as hemorrhage, infection, or surgical misadventure up to and including loss of the penis and death.[4][68]
- Intolerance or allergic reactions to the narcotics used.
- Especially in newborns, where the bodily pain reduction mechanisms are not yet fully developed, local anaesthesia is often insufficient for the operation. Even in conjunction with regional anaesthesia of the dorsal nerve of the penis, the rate of failure to provide sufficient anaesthetic even for experienced anaesthetists is still 5-10%. The general anaesthesia that would be needed for newborns, however, poses significant risks for the child, and, therefore, is only likely to be used in emergencies. A surgical operation without proper pain control can lead to the development of a specific pain memory[69]. In unsedated and partially sedated infants increased secretion of the stress hormone cortisol could be observed for months after the operation. Overall, their pain threshold was lower and the risk of chronic pain increased. Regardless of these findings, infant circumcisions with insufficient or no anaesthetic are still common practice[70][71][72]. During procedures which take several minutes, babies tend to fall into a state of stupor, which in the past was falsely interpreted as peaceful sleep, nurturing the belief that babies felt no pain. Measurements taken in those cases revealed a typically 3- to 4-fold increase in cortisol levels, which equals a state of severe shock.[73]
- Postoperative wound pain, in the case of children's circumcisions conceivably worsened by the forceful breaking of the preputial adhesions.
- Postoperative pain from the exposure of the sensitive glans penis to clothing. This pain will endure for several weeks or even longer in some cases.
- Postoperative bleeding of the wound. This can have severe consequences especially for very young infants, if they are not treated promptly. Their blood volume is only about 85 ml per kilogram of body weight, and even moderate blood loss can lead to hypovolaemia, hypovolaemic shock and even death.[74][75] [76][77]
- Post operative lymphoedema.
- Postoperative infections. This includes both local infections, which can be treated with local therapy, and systemic infections, requiring systemic antibiotic treatment.[78]
- Wound dehiscence, meaning the separation of the edges of the wound or the tissue after suturing.
- Adhesion between the surface or rim of the glans with the neighbouring penile skin, causing skin pockets and bridges, as well as visually unpleasant results like uneven scars, which make a re-circumcision necessary.
- Postoperative phimosis: a phimotic ring can develop during scarring, which makes a re-circumcision necessary. According to a study by Blalock et al.[79], the prevalence is 2.9%, according to Leitch[80] 5.5%.
- Sudden Infant Death Syndrome (SIDS).
- Knot formation of the veins. If the dorsal vein, which originates in the tip of the foreskin, is cut during circumcision without being clamped and sutured at its origin separately, it starts to develop new branches over time, which can lead to the development of knots.
- Possible deformities due to circumcision include hypoplasia of the penis (micro-penis) and induratio penis plastica (skewed penis).
- Medical malpractice can also not be ruled out. Injuries, partly or entirely severing the glans or the penis can occur.
- In rare cases, necrosis, gangrene, ischaemia, keloid formation, and circulatory problems may also occur.
- When the circumcision is followed by the ultra-orthodox Jewish ritual of Metzitzah B'Peh (which consists of sucking blood from the wound with the mouth), there is a risk of infection with herpes simplex type 1, which can lead to brain damage or death.[81]
Physical late effects
- An unavoidable late effect of any circumcision is the permanent loss of sexual sensitivity. This is partly due to the removal of sensory tissue. The foreskin contains very many nerve endings and touch receptors, which account for the major part of male sexual sensation. If the foreskin is removed, they can no longer provide sexual stimulation. It is also partly due to the fact that the surface of the glans reacts to the missing protection from friction and drying out by developing a callus layer. This reduces the sensitivity of the remaining nerves in the glans gradually over the years. The study conducted by Sorrells et al.[82] found a significant reduction of sensitivity to touch for circumcised compared to intact penises in adult males. Other studies revealed that circumcised men use condoms significantly less often than intact men, since they further limit the sexual sensitivity (see above).
- Painful tension can occur when there is too little reserve skin left to support a full erection[1]. This risk is partly dependent on the anatomy of the penis. While some penises already have the majority of their full size when flaccid (Flesh Penis, or "shower"), others are rather short when flaccid and double or more their size during an erection (Blood Penis, or "grower"). Especially in children's circumcision, where the penis is not yet fully developed, the amount of reserve skin needed in adulthood cannot be estimated.
- Erectile dysfunction: Both the damage inflicted to the blood vessels in the foreskin and the reduced sexual sensitivity can be causes for reduced erectile function with advancing age.[83]
- Orgasm problems: In the wake of reduced sexual sensitivity, due to the loss of sensory tissue and gradual keratinization of the surface of the glans, orgasm problems may develop with increasing age. In this case, the sexual arousal created by intercourse or masturbation is not enough to achieve orgasm. A preliminary stage of this late effect is the prolonged time circumcised] men need to reach an orgasm. This is often fielded as the "cut men have more endurance" argument for circumcision.
- Vaginal dryness: Due to the loss of the natural gliding action, which comes from the mobility of the foreskin and shaft skin, a much increased friction between penis and vagina occurs during intercourse. This can make intercourse painful for both partners and lead to abrasions[84][85] The prolonged time it takes circumcised men to reach orgasm, as well as the often longer and more vigorous thrusting movements - compared to intact men - play a part in this.[86][87]
- Lymphoedema of the penis is a normal and expected complication of male circumcision.
- Meatal stenosis, a pathological narrowing of the opening of the urethra, which mostly occurs in infancy and early childhood. It is one of the most common complications of infant circumcision. A study from 2006 found meatal stenosis exclusively in previously circumcised boys. The incidence rate after a circumcision is approximately 10 to 20 percent.[88][89][90]
- Shorter adult penile length was reported by Park et al. (2016) as a result of NMC (newborn male circumcision).
| “ | In conclusion, second to fourth digit ratio, flaccid penile length, and age of circumcision were significant predictive factors for erectile penile length. Furthermore, the penile lengths of the NMC group were shorter than those of the non-NMC group. – Park et al.[91] |
Sexual effects
Circumcision and frenectomy remove tissues with heightened erogenous sensitivity.[2] [92] They concluded, "Evidence has also started to accumulate that male circumcision may result in lifelong physical, sexual, and sometimes psychological harm as well."
The amputation of the prepuce results in the loss of the majority of fine-touch neuroreceptors found in the penis, leaving only the uninhibited protopathic sensibility of the artificially externalized glans penis. The imbalance caused by not having the input from the now ablated fine-touch receptors may be a leading cause of the changes in sexual behavior noted in circumcised human males.[93]
Histology of the male circumcision scar shows amputation neuromas, Schwann cell proliferation and the bulbous collection of variably sized neurites. Amputation neuromas do not mediate normal sensation and are notorious for generating pain.[86]
See Sexual effects of circumcision for more information.
Psychological effects
Psychological late effects are also possible after a circumcision, especially if the operation was carried out in childhood. On this occasion a variety of trauma may occur, which depend, among others, on age and circumstances of the circumcision. For example, whether the circumcision took place with or without sufficient anaesthesia, if the individual has been informed about the operation beforehand, if he was circumcised against his will or without his consent, and also, in the case of infant circumcision, if he was told about it during childhood or had to find it out coincidentally on his own.
The psychological late effects of circumcision are not yet fully researched, and many studies took place on rather a small scale. This situation needs to be rectified, because the available studies, as well as the histories of negatively affected men, suggest that these late effects may have more impact than previously assumed.
- It was observed that infants, following circumcision without pain control, had a disturbed bond with their mother[94], as well as problems with nurturing, up to the point of refusal to be fed. The sleeping habits of these babies were also disturbed, with prolonged non-REM sleep and increased waking.
- In boys circumcised in childhood, post-traumatic stress disorder (PTSD) could be diagnosed. In a study on Philippine boys, in whom no PTSD was found prior to the operation, 69% of the boys circumcised in the traditional ritual and 51% of those circumcised by standard medical procedures (including anaesthesia) fulfilled the DSM-IV criteria for PTSD following the operation.[95]
- Circumcisions, especially those that happen without consent, can spark feelings of helplessness and alienation, which can persist as trauma. These feeling can also be triggered later, when someone circumcised as an infant becomes aware of his circumcision. In an online study, interviewed men stated they felt betrayed - 55% by the mother, 50% by the father, and 58% by the doctor, and 73% felt that their human rights had been violated.[96]
- It can frequently be found that the loss is denied, much as happens with the loss of other body parts. This denial can lead to fathers having their sons circumcised in order not to be reminded of their own loss. In this process, their own body is defined as "normal" and the foreskin redefined as a foreign object. Their own parents are seen as "good", so that this image is projected onto the circumcision their parents carried out as well, in order to keep the positive emotion intact. The father wants to be a "good" father later in life as well, and so, following an idealised image of his own parents, circumcision, which has been redefined as a "good thing", is passed on to his son by having him circumcised as well.[97][98]
- If the circumcised male feels incomplete, or due to the missing foreskin disadvantaged compared to intact males, an inferiority complex and depression may occur. This can be accompanied by conscious recognition of his own incompleteness, or the deficiency may remain completely subconscious[99]. In an online study, 75% of those interviewed stated that they felt incomplete, and 66% said they felt inferior compared with intact males.[96]
- Cases in which children felt ill treated or punished have been documented as well. G. Cansever found in her study on 12 boys aged between 4 and 7 years, who had previously been prepared for their impending circumcision, that the children experienced the operation as an aggressive assault on their bodies.[100]
- Fear of being alone or darkness.[101]
- Fear of doctors, clinics and also closed rooms.[101]
- Relapse into the state of bed-wetting, even if the child was already dry before.[101]
- Circumcised males who become fathers frequently manifest adamant father syndrome.
Intact America (2019) called circumcision an adverse childhood experience,[102]
Complications
Death
A study in 2010 estimated approximately 117 neonatal circumcision-related deaths occur annually in the United States, about one out of every 77 male neonatal deaths, more than suffocation, auto accidents, or even SIDS.[103][104] See also the list of fatalities.
Forced circumcision
Non-therapeutic circumcision of male children
Human babies, because they are not yet in possession of language, are incapable of giving or refusing consent to be circumcised. The element of force has led some scholars to view the circumcision of baby boys as a category of forced circumcision.[105] There are, however, physicians in the United States who argue strongly for non-therapeutic circumcision of newborn babies; and circumcision is widely accepted as a postnatal procedure in American hospitals.[106] Parental consent is required.[107] A statement published by the American Academy of Pediatrics in 1999 claimed that "parents should determine what is in the best interest of the child... It is legitimate for parents to take into account cultural, religious, and ethnic traditions, in additions to the medical factors, when making a decision."[108] however surrogate consent for non-therapeutic circumcision is now viewed as unethical.
In the United Kingdom, where non-therapeutic circumcision has now become far less prevalent than in the United States, the written consent of both parents is required, if a physician is to perform a non-therapeutic circumcision of a child.[109] (The National Health Service does not provide non-therapeutic circumcision.)
In recent years, legal writers in several English-speaking countries have been questioning the practice of acceding to parental wishes.[110] For example, critics have pointed out that, in the United States, more than 1.3% of male neonatal deaths are attributable to the complications of non-therapeutic circumcision surgery.[103]
Video
Is circumcision healthy?
The video Is Circumcision Healthy is recommended for parental viewing.
Dr. Christopher Guest discusses circumcision
Plastibel circumcision
Stanford University has published a video of an actual non-therapeutic plastibell circumcision. The infant has received two injections of local anesthesia to deaden the dorsal nerves. The ventral nerves were not deadened so the infant still feels pain. One can his cries on the soundtrack.
Gomco clamp circumcision
Not for the squeamish:
This is a video of an actual circumcision with a Gomco clamp. The infant boy received two dorsal penile nerve block (DPNB) analgesic injections but they did not seem to work.
Recommendations of medical authorities
- Hill (2007) said:
Male circumcision is harmful because it excises healthy tissue and permanently impairs beneficial physiological functions. Male circumcision also causes psychological problems that tend to perpetuate the cycle of abuse. Male circumcision is a costly diversion of medical resources away from beneficial services. Male circumcision violates legal rights, human rights, and ethical standards. Finally, we must remember that males are the more vulnerable and sensitive of the two genders and, therefore, deserve the greater degree of protection from traumatic, invasive, injurious,and unnecessary surgery. For all of these reasons the non-therapeutic circumcision of boys should not be performed and the genital integrity of all children should be respected and protected.[111]
- Andrew E. MacNeiiy, Head, Division of Pediatric Urology, Department of Urological Sciences, University of British Columbia, Vancouver, BC, (2008) said:
Newborn circumcision remains an area of controversy. Social, cultural, aesthetic and religious pressures form the most common reasons for non-therapeutic circumcision. Although penile cancer and UTIs are reduced compared with uncircumcised males, the incidence of such illness is so low that circumcision cannot be justified as prophylaxis. The role of the foreskin in HIV transmission in developed countries is unclear, and safe sexual practice remains the cornerstone of prevention. There remains a lack of knowledge regarding what constitutes the normal foreskin both among parents and among primary care providers. This lack of knowledge results in a burden of costs to our health care system in the form of unnecessary urological referrals, expansion of wait times and circumcisions. Routine circumcision of all infants is not justified from a health or cost-benefit perspective.[112]
- The Royal Dutch Medical Association (KNMG) (2010) said:
The official viewpoint of KNMG and other related medical/scientific organisations is that non-therapeutic circumcision of male minors is a violation of children’s rights to autonomy and physical integrity. Contrary to popular belief, circumcision can cause complications – bleeding, infection, urethral stricture and panic attacks are particularly common. KNMG is therefore urging a strong policy of deterrence. KNMG is calling upon doctors to actively and insistently inform parents who are considering the procedure of the absence of medical benefits and the danger of complications.[113]
- The Royal Australasian College of Physicians (2010) said:
Ethical and human rights concerns have been raised regarding elective infant male circumcision because it is recognised that the foreskin has a functional role, the operation is non-therapeutic and the infant is unable to consent.
After reviewing the currently available evidence, the RACP believes that the frequency of diseases modifiable by circumcision, the level of protection offered by circumcision and the complication rates of circumcision do not warrant routine infant circumcision in Australia and New Zealand. However it is reasonable for parents to weigh the benefits and risks of circumcision and to make the decision whether or not to circumcise their sons.[114]
- The American Academy of Pediatrics (AAP) has not re-affirmed its disastrous, failed 2012 Circumcision Policy Statement, which expired in 2017, so currently has no position on child circumcision.
- Medical historian Robert Darby (2014) wrote simply:
"To avoid circumcision complications, avoid circumcision."[115]
- The Canadian Paediatric Society (CPS) (2015) said:
In most jurisdictions, authority is limited only to interventions deemed to be medically necessary. In cases in which medical necessity is not established or a proposed treatment is based on personal preference, interventions should be deferred until the individual concerned is able to make their own choices.[116]
- The Canadian Urological Association (CUA) considered the matter of circumcision and issued a statement in February 2018. The CUA concluded:
"Given the socioeconomic, educational status, and health demographics of our population, universal neonatal circumcision cannot be justified based on the current evidence available.[117]
British family court opinion
The issue of non-therapeutic circumcision of male children came before the court in the case of Re B and G (children) (No 2) EWFC 3 (2015) . In that case, Judge Sir James Munby ruled that circumcision of male children caused significant harm.
Rights and ethics
The rights situation is discussed in a separate article.
The term "circumcision" without a gender qualifier refers specifically to male circumcision. It means "to cut around," and it refers to the excision of the foreskin from the penis. The term is inaccurate and a euphemism because the operation actually cuts off or amputates the foreskin, which in adults comprises about fifteen square inches of highly functional erogenous tissue.
Circumcision is most often performed in healthy males for religious or cultural reasons. The procedure may be performed on consenting adults, but it is most often performed on non-consenting minors, particularly newborn children, which is why the ritual is so controversial. Opponents of circumcision consider the circumcision of non-consenting minors to be unethical and a human rights violation, unless there is concrete medical indication.
Consent by surrogates
Medical ethics has long recognized limitations on the power of consent by surrogates.[118] [119] [120]
Two ethicists, Myers & Earp (2020), have conducted a detailed review and analysis of the claimed medical benefits of non-therapeutic circumcision. They have determined than the alleged benefits are not material, so they do not support granting of consent by a surrogate. In other words, Non-therapeutic circumcision is not truly healthcare. Moreover, they comment that even the most perfectly executed surgery produces trauma and harm to the patient. Circumcision also produces tissue loss and loss of function, therefore, circumcision should be performed only after the individual reaches the age of consent. Consent by a surrogate for a non-therapeutic circumcision of a minor child is an unethical practice.[121]
See also
- Adolescent and adult circumcision
- Breastfeeding
- Case Histories
- Circumcision maps
- Circumcision methods
- Circumcision scar
- Circumpendium
- Circumstraint
- Documented severe complications of circumcision
- Ethics of non-therapeutic child circumcision
- FGM
- Human rights
- Lymphoedema
- MGM
- Pain
- Psychological issues of male circumcision
- Rights situation on circumcision
- Risks and complications
- Sexual effects of circumcision
- Sudden Infant Death Syndrome (SIDS)
- Trauma
External links
 Garcia, Francisco (11 December 1995).
Garcia, Francisco (11 December 1995). What exactly is circumcision and what is it not?
. Retrieved 8 September 2020. Fleiss P. The foreskin is necessary. Mothering. January 1997; : 36-45. Retrieved 29 June 2020.
Fleiss P. The foreskin is necessary. Mothering. January 1997; : 36-45. Retrieved 29 June 2020. Ball, Peter (9 August 2003).
Ball, Peter (9 August 2003). Losses from Circumcision
, 15 Square. Retrieved 23 February 2023. Winkel, Rich (12 May 2005).
Winkel, Rich (12 May 2005). Male Circumcision in the USA: A Human Rights Primer
. Retrieved 27 January 2021.
 Testa, Patrick, Block, Walter E.. Libertarianism and circumcision. Int J Health Poiicy Manag. 26 May 2014; 3: 33-40. PMID. PMC. DOI.
Testa, Patrick, Block, Walter E.. Libertarianism and circumcision. Int J Health Poiicy Manag. 26 May 2014; 3: 33-40. PMID. PMC. DOI.
 Simone, Judy (26 July 2020).
Simone, Judy (26 July 2020). What is circumcision?
, https://intaction.org/, Intaction. Retrieved 4 October 2020. Deacon M, Muir G. What is the medical evidence on non-therapeutic child circumcision?. Int J Impot Res. 8 January 2022; PMID. DOI. Retrieved 30 April 2023.
Deacon M, Muir G. What is the medical evidence on non-therapeutic child circumcision?. Int J Impot Res. 8 January 2022; PMID. DOI. Retrieved 30 April 2023.
References
- ↑ a b c
 Taylor JR, Lockwood AP, Taylor AJ. The prepuce: specialized mucosa of the penis and its loss to circumcision. Br J Urol. 1996; 77: 291-5. PMID. DOI. Retrieved 23 September 2019.
Taylor JR, Lockwood AP, Taylor AJ. The prepuce: specialized mucosa of the penis and its loss to circumcision. Br J Urol. 1996; 77: 291-5. PMID. DOI. Retrieved 23 September 2019.
- ↑ a b
 Cepeda-Emiliani A, Gándara-Cortés M, Otero-Alén M, García H, Suárez-Quintanilla J, García-Caballero T, Gallego R, García-Caballero R. Immunohistological study of the density and distribution of human penile neural tissue: gradient hypothesis. Int J Impot Res. 2 May 2023; 35(3): 286-305. PMID. DOI. Retrieved 23 November 2023.
Cepeda-Emiliani A, Gándara-Cortés M, Otero-Alén M, García H, Suárez-Quintanilla J, García-Caballero T, Gallego R, García-Caballero R. Immunohistological study of the density and distribution of human penile neural tissue: gradient hypothesis. Int J Impot Res. 2 May 2023; 35(3): 286-305. PMID. DOI. Retrieved 23 November 2023.
- ↑
 Bollinger D. Adverse Childhood Experiences, Dysfunctional Households, And Circumcision.. Kindred. 28 February 2023; Retrieved 1 March 2023.
Bollinger D. Adverse Childhood Experiences, Dysfunctional Households, And Circumcision.. Kindred. 28 February 2023; Retrieved 1 March 2023.
- ↑ a b
 Deacon M, Muir G. What is the medical evidence on non-therapeutic child circumcision?. Int J Impot Res. 8 January 2022; PMID. DOI. Retrieved 30 January 2022.
Deacon M, Muir G. What is the medical evidence on non-therapeutic child circumcision?. Int J Impot Res. 8 January 2022; PMID. DOI. Retrieved 30 January 2022.
- ↑
 DeMeo (1997): The geography of sexual mutilations. Work: Sexual Mutilations: A Human Tragedy. George C. Denniston, Marilyn Milos (eds.). New York: Plenum. ISBN 0-306-45589-7. Retrieved 13 November 2021.
DeMeo (1997): The geography of sexual mutilations. Work: Sexual Mutilations: A Human Tragedy. George C. Denniston, Marilyn Milos (eds.). New York: Plenum. ISBN 0-306-45589-7. Retrieved 13 November 2021.
- ↑

File:Circumcision Sakkara 3.jpg
. Retrieved 12 October 2019. - ↑
 Luke.
Luke. Gospel of Luke
, Bible Gateway, NASB. Retrieved 10 November 2019.
Quote:And when eight days had passed, before His circumcision, His name was then called Jesus, the name given by the angel before He was conceived in the womb.
- ↑
 Luke.
Luke. Acts 15:1-30
. Retrieved 10 November 2019. - ↑
 Hill, George (29 August 2004).
Hill, George (29 August 2004). The Holy Bible, Circumcision, False Prophets, and Christian Parents
 , Circumcision Reference Library. Retrieved 10 November 2019.
, Circumcision Reference Library. Retrieved 10 November 2019.
Quote:The falseness of those who advocate circumcision is a recurrent theme in the New Testament.
- ↑
 Kellogg JH (1888):
Kellogg JH (1888): Treatment for Self-abuse and Its Effects
, in: Plain Facts for Old and Young. Burlington, Iowa: F. Segner & Co.. P. 107. - ↑
 Cheyne, T. K. (1876).
Cheyne, T. K. (1876). Circumcision
, Circumcision Reference Library, Encyclopǽdia Brittanica. Retrieved 10 November 2019. - ↑
 Cold C, McGrath K (1999):
Cold C, McGrath K (1999): Anatomy and histology of the penile and clitoral prepuce in primates
, in: Male and female circumcision: medical, legal, and ethical considerations in pediatric practice. New York ISBN 0306461315. Retrieved 12 October 2019. - ↑
 Anonymous (2016).
Anonymous (2016). Conclusions
, Doctors Opposing Circumcision. Retrieved 22 October 2023. - ↑
 Ephron JM (2001):
Ephron JM (2001): 6
, in: Medicine and the German Jews. New Haven: Yale University Press. Pp. 222-33. ISBN 0-300-08377-7. Retrieved 20 November 2019. - ↑ https://nypost.com/2016/12/03/bellevues-doctors-invented-the-procedures-you-take-for-granted/
- ↑ American Medical Association. Transactions of the American Medical Association. 1870;21:205–11
- ↑
 Wolbarst AL. Is circumcision a prophylactic against penis cancer?. Cancer. July 1926; 3(4): 301-10.
Wolbarst AL. Is circumcision a prophylactic against penis cancer?. Cancer. July 1926; 3(4): 301-10.
- ↑
 Hand EH. Circumcision and venereal disease. Archives of Dermatology and Syphilology. September 1949; 60(3) PMID. DOI. Retrieved 8 October 2021.
Hand EH. Circumcision and venereal disease. Archives of Dermatology and Syphilology. September 1949; 60(3) PMID. DOI. Retrieved 8 October 2021.
- ↑
 Ravich A. Prophylaxis of cancer of the prostate, penis, and cervix by circumcision. New York State Journal of Medicine. June 1951; 51(12): 1519-20. PMID. Retrieved 6 October 2021.
Ravich A. Prophylaxis of cancer of the prostate, penis, and cervix by circumcision. New York State Journal of Medicine. June 1951; 51(12): 1519-20. PMID. Retrieved 6 October 2021.
- ↑
 Fishbein M (1969):
Fishbein M (1969): Sex hygiene
, in: Modern Home Medical Adviser. Garden City (ed.). New York: Doubleday & Co. Pp. 90+119. Retrieved 30 October 2021. - ↑
 Ravich A. Viral carcinogenesis in venereally susceptible organs. Cancer. June 1971; 27(6): 1493-6. Retrieved 12 October 2019.
Ravich A. Viral carcinogenesis in venereally susceptible organs. Cancer. June 1971; 27(6): 1493-6. Retrieved 12 October 2019.
- ↑
 Wiswell TE. Decreased incidence of urinary tract infections in circumcised male infants. Pediatrics. May 1985; 75(5): 901-3. Retrieved 12 October 2019.
Wiswell TE. Decreased incidence of urinary tract infections in circumcised male infants. Pediatrics. May 1985; 75(5): 901-3. Retrieved 12 October 2019.
- ↑
 Fink AJ. A possible explanation for heterosexual male infection with AIDS. New England Journal of Medicine. 30 October 1986; 31(18): 1167. DOI. Retrieved 20 November 2019.
Fink AJ. A possible explanation for heterosexual male infection with AIDS. New England Journal of Medicine. 30 October 1986; 31(18): 1167. DOI. Retrieved 20 November 2019.
- ↑
 (May 2016).
(May 2016). Alleged Medical Benefits
, Doctors Opposing Circumcision (D.O.C.). Retrieved 20 November 2019. - ↑
 Blalock HJ, Vemulakonda V, Ritchey ML, Ribbeck M. Outpatient management of phimosis Following newborn circumcision. J Urol. 2003; 169(6): 2332-4. Retrieved 7 November 2019.
Blalock HJ, Vemulakonda V, Ritchey ML, Ribbeck M. Outpatient management of phimosis Following newborn circumcision. J Urol. 2003; 169(6): 2332-4. Retrieved 7 November 2019.
- ↑
 Laumann EO, Masi CM, Zuckerman EW. Circumcision in the United States: prevalence, prophylactic effects, and sexual practice. JAMA. 1997; 277: 1052-7. Retrieved 6 November 2019.
Laumann EO, Masi CM, Zuckerman EW. Circumcision in the United States: prevalence, prophylactic effects, and sexual practice. JAMA. 1997; 277: 1052-7. Retrieved 6 November 2019.
- ↑ a b
 Fleiss P, Hodges F, Van Howe RS. Immunological functions of the human prepuce. Sex Trans Infect. October 1998; 74(5): 364-67. PMID. PMC. DOI. Retrieved 14 January 2022.
Fleiss P, Hodges F, Van Howe RS. Immunological functions of the human prepuce. Sex Trans Infect. October 1998; 74(5): 364-67. PMID. PMC. DOI. Retrieved 14 January 2022.
- ↑
 Task Force on Circumcision. Circumcision policy statement. Pediatrics. 1999; 103(3): 686-93. Retrieved 15 November 2019.
Task Force on Circumcision. Circumcision policy statement. Pediatrics. 1999; 103(3): 686-93. Retrieved 15 November 2019.
- ↑
 Hooykaas C, van der Velde FW, van der Linden MM, et al. The importance of ethnicity as a risk factor for STDs and sexual behaviour among heterosexuals. Genitourin Med. 1991; 67(5): 378-83. Retrieved 15 November 2019.
Hooykaas C, van der Velde FW, van der Linden MM, et al. The importance of ethnicity as a risk factor for STDs and sexual behaviour among heterosexuals. Genitourin Med. 1991; 67(5): 378-83. Retrieved 15 November 2019.
- ↑
 Michael RT, Wadsworth J, Feinleib J, et al. Private sexual behavior, public opinion, and public health policy related to sexually transmitted diseases: a US-British comparison. Am J Public Health. 1998; 88(5): 749-54. Retrieved 15 November 2019.
Michael RT, Wadsworth J, Feinleib J, et al. Private sexual behavior, public opinion, and public health policy related to sexually transmitted diseases: a US-British comparison. Am J Public Health. 1998; 88(5): 749-54. Retrieved 15 November 2019.
- ↑
 Laumann EO, Masi CM, Zuckerman EW. Circumcision in the United States: prevalence, prophylactic effects, and sexual practice. JAMA. 1997; 277: 1052-7. Retrieved 6 November 2019.
Laumann EO, Masi CM, Zuckerman EW. Circumcision in the United States: prevalence, prophylactic effects, and sexual practice. JAMA. 1997; 277: 1052-7. Retrieved 6 November 2019.
- ↑
 Gray RH, Kigozi G, Serwadda D, et al. Male circumcision for HIV prevention in men in Rakai, Uganda: A randomised trial. Lancet. 24 February 2007; 369(9562): 657-66. PMID. DOI. Retrieved 31 December 2021.
Gray RH, Kigozi G, Serwadda D, et al. Male circumcision for HIV prevention in men in Rakai, Uganda: A randomised trial. Lancet. 24 February 2007; 369(9562): 657-66. PMID. DOI. Retrieved 31 December 2021.
- ↑
 Bailey RC, Moses S, Parker CB, et al. Male circumcision for HIV prevention in young men in Kisumu, Kenya: A randomised controlled trial. Lancet. 24 February 2007; 369(9562): 643–56. PMID. DOI. Retrieved 31 December 2021.
Bailey RC, Moses S, Parker CB, et al. Male circumcision for HIV prevention in young men in Kisumu, Kenya: A randomised controlled trial. Lancet. 24 February 2007; 369(9562): 643–56. PMID. DOI. Retrieved 31 December 2021.
- ↑
 Boyle GJ, Hill G. Sub-Saharan African randomised clinical trials into male circumcision and HIV transmission: Methodological, ethical and legal concerns
Boyle GJ, Hill G. Sub-Saharan African randomised clinical trials into male circumcision and HIV transmission: Methodological, ethical and legal concerns  . Thompson Reuter. December 2011; 19(2): 316-34. PMID. Retrieved 30 December 2020.
. Thompson Reuter. December 2011; 19(2): 316-34. PMID. Retrieved 30 December 2020.
- ↑
 Grosskurth H, Mosha F, Todd J, et al. A community trial of the impact of improved sexually transmitted disease treatment on the HIV epidemic in rural Tanzania: 2. Baseline survey results. AIDS. 1995; 9(8): 927-34. Retrieved 15 November 2019.
Grosskurth H, Mosha F, Todd J, et al. A community trial of the impact of improved sexually transmitted disease treatment on the HIV epidemic in rural Tanzania: 2. Baseline survey results. AIDS. 1995; 9(8): 927-34. Retrieved 15 November 2019.
- ↑
 Barongo LR, Borgdorff MW, Mosha FF, et al. The epidemiology of HIV-1 infection in urban areas, roadside settlements and rural villages in Mwanza Region, Tanzania. AIDS. 1992; 6(12): 1521-8.
Barongo LR, Borgdorff MW, Mosha FF, et al. The epidemiology of HIV-1 infection in urban areas, roadside settlements and rural villages in Mwanza Region, Tanzania. AIDS. 1992; 6(12): 1521-8.
- ↑
 Changedia SM, Gilada IS: Role of male circumcision in HIV transmission insignificant in conjugal relationship (abstract no. ThPeC7420), Barcelona, Spain. (7 July 2002–12 July 2002) Presented at the Fourteenth International AIDS Conference.
Changedia SM, Gilada IS: Role of male circumcision in HIV transmission insignificant in conjugal relationship (abstract no. ThPeC7420), Barcelona, Spain. (7 July 2002–12 July 2002) Presented at the Fourteenth International AIDS Conference.
- ↑
 Connolly CA, Shishana O, Simbayi L, Colvin M: HIV and circumcision in South Africa (Abstract No. MoPeC3491), Bangkok, Thailand. (11 July 2004–16 July 2004) Presented at the 15th International AIDS Conference.
Connolly CA, Shishana O, Simbayi L, Colvin M: HIV and circumcision in South Africa (Abstract No. MoPeC3491), Bangkok, Thailand. (11 July 2004–16 July 2004) Presented at the 15th International AIDS Conference.
- ↑
 Thomas AG, Bakhireva LN, Brodine SK, Shaffer RA: Prevalence of male circumcision and its association with HIV and sexually transmitted infections in a U.S. navy population (Abstract no. TuPeC4861), Bangkok, Thailand. (11 July 2004–16 July 2004) Presented at the 15th International AIDS Conference. Retrieved 15 November 2019.
Thomas AG, Bakhireva LN, Brodine SK, Shaffer RA: Prevalence of male circumcision and its association with HIV and sexually transmitted infections in a U.S. navy population (Abstract no. TuPeC4861), Bangkok, Thailand. (11 July 2004–16 July 2004) Presented at the 15th International AIDS Conference. Retrieved 15 November 2019.
- ↑
 McCracken G. Options in antimicrobial management of urinary tract infections in infants and children. Pediatr Infect Dis J. 1989; 8(8): 552-5. Retrieved 19 November 2019.
McCracken G. Options in antimicrobial management of urinary tract infections in infants and children. Pediatr Infect Dis J. 1989; 8(8): 552-5. Retrieved 19 November 2019.
- ↑
 Larcombe J. Urinary tract infection in children. BMJ. 1999; 319: 1173-5.
Larcombe J. Urinary tract infection in children. BMJ. 1999; 319: 1173-5.
- ↑
 Mårild S, Jodal U. Incidence rate of first–time symptomatic urinary tract infection in children under 6 years of age. Acta Paediatr. 1998; 87(5): 549-52.
Mårild S, Jodal U. Incidence rate of first–time symptomatic urinary tract infection in children under 6 years of age. Acta Paediatr. 1998; 87(5): 549-52.
- ↑
 Mueller ER, Steinhardt G, Naseer S. The incidence of genitourinary abnormalities in circumcised and uncircumcised boys presenting with an initial urinary tract infection by 6 months of age. Pediatrics. 1997; 100 (Supplement): 580.
Mueller ER, Steinhardt G, Naseer S. The incidence of genitourinary abnormalities in circumcised and uncircumcised boys presenting with an initial urinary tract infection by 6 months of age. Pediatrics. 1997; 100 (Supplement): 580.
- ↑
 Menahem S. Complications arising from ritual circumcision: pathogenesis and possible prevention. Isr J Med Sci. 1981; 17(1): 45-8.
Menahem S. Complications arising from ritual circumcision: pathogenesis and possible prevention. Isr J Med Sci. 1981; 17(1): 45-8.
- ↑
 Cohen HA, Drucker MM, Vainer S, et al. Postcircumcision urinary tract infection. Clin Pediatr. 1992; 31(6): 322-4.
Cohen HA, Drucker MM, Vainer S, et al. Postcircumcision urinary tract infection. Clin Pediatr. 1992; 31(6): 322-4.
- ↑
 Goldman M, Barr J, Bistritzer T, Aladjem M. Urinary tract infection following ritual Jewish circumcision. Isr J Med Sci. 1996; 32: 1098-1102.
Goldman M, Barr J, Bistritzer T, Aladjem M. Urinary tract infection following ritual Jewish circumcision. Isr J Med Sci. 1996; 32: 1098-1102.
- ↑
 Wolbarst AL. Circumcision and penile cancer. Lancet. 16 January 1932; 1(5655): 150-3. DOI. Retrieved 13 March 2022.
Wolbarst AL. Circumcision and penile cancer. Lancet. 16 January 1932; 1(5655): 150-3. DOI. Retrieved 13 March 2022.
- ↑
 McCance DJ, Kalache A, Ashdown K, et al. Human papillomavirus types 16 and 18 in carcinomas of the penis from Brazil. Int J Cancer. 1986; 37(1): 55-9.
McCance DJ, Kalache A, Ashdown K, et al. Human papillomavirus types 16 and 18 in carcinomas of the penis from Brazil. Int J Cancer. 1986; 37(1): 55-9.
- ↑
 Harish K, Ravi R. The role of tobacco in penile carcinoma. Brit J Urol. 1995; 75(3): 375-7.
Harish K, Ravi R. The role of tobacco in penile carcinoma. Brit J Urol. 1995; 75(3): 375-7.
- ↑
 Position Paper on Neonatal Circumcision, American Academy of Family Physicians (Leawood, Kansas). (14 February 2002).
Position Paper on Neonatal Circumcision, American Academy of Family Physicians (Leawood, Kansas). (14 February 2002).
- ↑
 Persad R, Sharma S, McTavish J, et al. Clinical presentation and pathophysiology of meatal stenosis following circumcision. Brit J Urol. 1995; 75(1): 91-3. PMID. DOI. Retrieved 26 November 2019.
Persad R, Sharma S, McTavish J, et al. Clinical presentation and pathophysiology of meatal stenosis following circumcision. Brit J Urol. 1995; 75(1): 91-3. PMID. DOI. Retrieved 26 November 2019.
- ↑
 Anand, Hickey. Pain and its effects in the human neonate and fetus. New Engl J Med. 19 November 1987; 317(21): 1321-9. PMID. Retrieved 8 November 2019.
Anand, Hickey. Pain and its effects in the human neonate and fetus. New Engl J Med. 19 November 1987; 317(21): 1321-9. PMID. Retrieved 8 November 2019.
- ↑
 American Academy of Pediatrics: Circumcision Policy Statement; Task Force on Circumcision. Pediatrics. March 1999; 103(3): 686-93. Retrieved 26 November 2019.
American Academy of Pediatrics: Circumcision Policy Statement; Task Force on Circumcision. Pediatrics. March 1999; 103(3): 686-93. Retrieved 26 November 2019.
- ↑

Circumcision: Position Paper on Neonatal Circumcision. Board Approved: August 2007 Reaffirmed
, Official American Academy of Family Physicians Website. Retrieved 2 May 2011. - ↑

Report 10 of the Council on Scientific Affairs (I-99): Neonatal Circumcision
, American Medical Association Official Website. Retrieved 4 May 2011. - ↑
 (23 March 2011).
(23 March 2011). Where We Stand: Circumcision
, AAP. Retrieved 12 October 2019. - ↑

Parents' Guide to Circumcision
. Retrieved 8 April 2011.
Quote:To calm the baby during the procedure, a sugar filled gauze pacifier soaked with sweet juice is used, and soothing music is played in the room.
- ↑
 (8 April 2011).
(8 April 2011). Before the Circumcision
. Retrieved 8 April 2011.
Quote:During the circumcision, your son will receive sugar pacifiers to suck on which reduce his pain perceptions.
- ↑
 (8 April 2011).
(8 April 2011). Before the Circumcision
. Retrieved 8 April 2011.
Quote:Then in our office, he will have topical anesthetic applied to his penis.
- ↑

Parents' Guide to Circumcision
. Retrieved 8 April 2011.
Quote:We use extensive pain control methods including Tylenol, a sugar solution (to reduce pain perceptions), a topical freezing cream, and a local anesthetic injection.
- ↑
 Taeusch HW, Martinez AM, Partridge JC, Sniderman S, Armstrong-Wells J, Fuentes-Afflick E. Pain During Mogen or Plastibell Circumcision. Journal of Perinatology. April 2002; 22(3): 214-8. Retrieved 8 April 2011.
Taeusch HW, Martinez AM, Partridge JC, Sniderman S, Armstrong-Wells J, Fuentes-Afflick E. Pain During Mogen or Plastibell Circumcision. Journal of Perinatology. April 2002; 22(3): 214-8. Retrieved 8 April 2011.
Quote:...more than half of the study group had what we considered excessive pain/discomfort over the course of the entire procedure.
- ↑
 Williamson PS, Evans ND. Neonatal Cortisol Response to Circumcision with Anesthesia. Clinical Pediatrics. August 1986; 25(8): 412-6. Retrieved 8 April 2011.
Williamson PS, Evans ND. Neonatal Cortisol Response to Circumcision with Anesthesia. Clinical Pediatrics. August 1986; 25(8): 412-6. Retrieved 8 April 2011.
Quote:The adrenal cortisol response to surgery was not significantly reduced by the administration of lidocaine.
- ↑
 (8 April 2011).
(8 April 2011). Before the Circumcision
. Retrieved 8 April 2011.
Quote:During the circumcision, your son will receive sugar pacifiers to suck on which reduce his pain perceptions.
- ↑
 Slater R, Cornelissen L, Fabrizi L, Patten D, Yoxen J, Worley A, Boyd S, Meek J, Prof. Fitzgerald M. Oral sucrose as an analgesic drug for procedural pain in newborn infants: a randomised controlled trial. The Lancet. 9 October 2010; 376(9748): 1225-32. Retrieved 8 April 2011.
Slater R, Cornelissen L, Fabrizi L, Patten D, Yoxen J, Worley A, Boyd S, Meek J, Prof. Fitzgerald M. Oral sucrose as an analgesic drug for procedural pain in newborn infants: a randomised controlled trial. The Lancet. 9 October 2010; 376(9748): 1225-32. Retrieved 8 April 2011.
Quote:Our data suggest that oral sucrose does not significantly affect activity in neonatal brain or spinal cord nociceptive circuits, and therefore might not be an effective analgesic drug. The ability of sucrose to reduce clinical observational scores after noxious events in newborn infants should not be interpreted as pain relief.
- ↑
 Taddio A, Goldbach M, Ipp M, Stevens B, Koren G. Effect of neonatal circumcision on pain responses during vaccination in boys. Lancet. 1995; 345: 291-292. PMC. DOI. Retrieved 15 November 2022.
Taddio A, Goldbach M, Ipp M, Stevens B, Koren G. Effect of neonatal circumcision on pain responses during vaccination in boys. Lancet. 1995; 345: 291-292. PMC. DOI. Retrieved 15 November 2022.
- ↑
 Taddio A, Katz J, Ilersich AL, Koren G. Effect of neonatal circumcision on pain response during subsequent routine vaccination. Lancet. 1 March 1997; 349: 599-603. PMC. DOI. Retrieved 15 November 2022.
Taddio A, Katz J, Ilersich AL, Koren G. Effect of neonatal circumcision on pain response during subsequent routine vaccination. Lancet. 1 March 1997; 349: 599-603. PMC. DOI. Retrieved 15 November 2022.
- ↑
 Uberoi M, Abdulcadir J, Ohi DA, Santiago JE, et al. Potentially under-recognized late-stage physical and psychosexual complications of non-therapeutic neonatal penile circumcision: a qualitative and quantitative analysis of self-reports from an online community forum. Int J Impot Res. 23 October 2022; PMID. DOI. Retrieved 8 January 2023.
Uberoi M, Abdulcadir J, Ohi DA, Santiago JE, et al. Potentially under-recognized late-stage physical and psychosexual complications of non-therapeutic neonatal penile circumcision: a qualitative and quantitative analysis of self-reports from an online community forum. Int J Impot Res. 23 October 2022; PMID. DOI. Retrieved 8 January 2023.
- ↑
 Williams N, Kapilla L. Complications of circumcision. Brit J Surg. October 1993; 80(10): 1231-6. PMID. DOI. Retrieved 27 November 2019.
Williams N, Kapilla L. Complications of circumcision. Brit J Surg. October 1993; 80(10): 1231-6. PMID. DOI. Retrieved 27 November 2019.
- ↑
 Prof. Dr. med. Boris Zernikow (12 August 2012).
Prof. Dr. med. Boris Zernikow (12 August 2012). Kinderschmerz-Experte warnt: Rituelle Beschneidung verändert das Gehirn der Kinder
[Children's pain expert warns: Ritual circumcision changes the brain of children] (German), Spiegel Online. Retrieved 11 October 2019. - ↑
 Garry T. Circumcision: a survey of fees and practices. OBG Management. 1994; October: 34-6.
Garry T. Circumcision: a survey of fees and practices. OBG Management. 1994; October: 34-6.
- ↑
 Howard CR, Howard FM, Garfunkel LC, de Blieck EA, Weitzman M. Neonatal circumcision and pain relief: current training practices. Pediatrics. 1998; 101: 423-8.
Howard CR, Howard FM, Garfunkel LC, de Blieck EA, Weitzman M. Neonatal circumcision and pain relief: current training practices. Pediatrics. 1998; 101: 423-8.
- ↑
 Stang HJ, Snellman LW. Circumcision practice patterns in the United States. Pediatrics. 1998; 101(e5)
Stang HJ, Snellman LW. Circumcision practice patterns in the United States. Pediatrics. 1998; 101(e5)
- ↑
 Gunnar MR, Fisch RO, Korsvik S, Donhowe JM. The effects of circumcision on serum cortisol and behavior. Psychoneuroendocrinology. 1981; 6(3): 269-75. Retrieved 26 November 2019.
Gunnar MR, Fisch RO, Korsvik S, Donhowe JM. The effects of circumcision on serum cortisol and behavior. Psychoneuroendocrinology. 1981; 6(3): 269-75. Retrieved 26 November 2019.
- ↑
 (2000) Paediatric Handbook. Smart J, Nolan T. (eds.). Edition: 6. VIC, Australia: Blackwell Science Asia. P. 82.
(2000) Paediatric Handbook. Smart J, Nolan T. (eds.). Edition: 6. VIC, Australia: Blackwell Science Asia. P. 82.
- ↑
 Wetli, CV: Autopsy of Demetrius Manker, Contribution:
Wetli, CV: Autopsy of Demetrius Manker, Contribution: Case 93-1711
, Miami: Dade County Medical Examiner Department. (23 June 1993). - ↑
 Hiss J, Horowitz A, Kahana T. Fatal haemorrhage following male ritual circumcision. J Clin Forensic Med. 2000; 7: 32-4. Retrieved 6 November 2019.
Hiss J, Horowitz A, Kahana T. Fatal haemorrhage following male ritual circumcision. J Clin Forensic Med. 2000; 7: 32-4. Retrieved 6 November 2019.
- ↑
 Newell, TEC: Judgement of inquiry into the death of McWillis, Ryleigh Roman Bryan, Burnaby, B.C.: B.C. Coroner's Service. (19 January 2004). Retrieved 26 November 2019.
Newell, TEC: Judgement of inquiry into the death of McWillis, Ryleigh Roman Bryan, Burnaby, B.C.: B.C. Coroner's Service. (19 January 2004). Retrieved 26 November 2019.
- ↑
 Dr. med. Hartmann, Wolfgang: Stellungnahme zur Anhörung am 26. November 2012 [Opinion on the hearing on 26 November 2012] (German), Rechtsausschuss des Bundestages [Legal Committee of the Bundestag] (German). (26 November 2012)
Dr. med. Hartmann, Wolfgang: Stellungnahme zur Anhörung am 26. November 2012 [Opinion on the hearing on 26 November 2012] (German), Rechtsausschuss des Bundestages [Legal Committee of the Bundestag] (German). (26 November 2012)
- ↑
 Blalock HJ, Vemulakonda V, Ritchey ML, Ribbeck M. Outpatient management of phimosis Following newborn circumcision. J Urol. 2003; 169(6): 2332-4. Retrieved 26 November 2019.
Blalock HJ, Vemulakonda V, Ritchey ML, Ribbeck M. Outpatient management of phimosis Following newborn circumcision. J Urol. 2003; 169(6): 2332-4. Retrieved 26 November 2019.
- ↑
 Leitch IOW. Circumcision - a continuing enigma. Aust Paediatr J. 1970; 6: 59-65. Retrieved 15 December 2019.
Leitch IOW. Circumcision - a continuing enigma. Aust Paediatr J. 1970; 6: 59-65. Retrieved 15 December 2019.
- ↑
 Robbins, Liz (7 March 2012).
Robbins, Liz (7 March 2012). Baby’s Death Renews Debate Over a Circumcision Ritual
. Retrieved 11 October 2019. - ↑
 Sorrells ML, Snyder JL, Reiss MD, Eden C, Milos MF, Wilcox N, Van Howe RS. Fine‐touch pressure thresholds in the adult penis. BJUI. 19 March 2007; 99(4): 864-9. PMID. DOI. Retrieved 10 January 2021.
Sorrells ML, Snyder JL, Reiss MD, Eden C, Milos MF, Wilcox N, Van Howe RS. Fine‐touch pressure thresholds in the adult penis. BJUI. 19 March 2007; 99(4): 864-9. PMID. DOI. Retrieved 10 January 2021.
- ↑
 Money J, Davison J. Adult penile circumcision: Erotosexual and cosmetic sequelae. Journal of Sex Research. 1983; 19: 289-92.
Money J, Davison J. Adult penile circumcision: Erotosexual and cosmetic sequelae. Journal of Sex Research. 1983; 19: 289-92.
- ↑
 Frisch M, Lindholm M, Grønbæk M. Male circumcision and sexual function in men and women: a survey-based, cross-sectional study in Denmark. Int J Epidemiol. 14 June 2011; 40(5): 1367-81. PMID. DOI. Retrieved 26 September 2021.
Frisch M, Lindholm M, Grønbæk M. Male circumcision and sexual function in men and women: a survey-based, cross-sectional study in Denmark. Int J Epidemiol. 14 June 2011; 40(5): 1367-81. PMID. DOI. Retrieved 26 September 2021.
- ↑
 Cortés-González J, Arratia-Maqueo J, Gómez-Guerra L. Does circumcision has an effect on female's perception of sexual satisfaction?. Rev Invest Clin. 2008; 60(3): 227. PMID.
Cortés-González J, Arratia-Maqueo J, Gómez-Guerra L. Does circumcision has an effect on female's perception of sexual satisfaction?. Rev Invest Clin. 2008; 60(3): 227. PMID.
- ↑ a b
 Cold CJ, Taylor JR. The prepuce. BJU Int. January 1999; 83, Suppl. 1: 34-44. PMID. DOI. Retrieved 8 July 2021.
Cold CJ, Taylor JR. The prepuce. BJU Int. January 1999; 83, Suppl. 1: 34-44. PMID. DOI. Retrieved 8 July 2021.
- ↑
 Fink KS, Carson CC, DeVellis RF. Adult Circumcision Outcomes Study: Effect on Erectile Function, Penile Sensitivity, Sexual Activity and Satisfaction. J Urol. 2002; 167(5): 2113-6.
Fink KS, Carson CC, DeVellis RF. Adult Circumcision Outcomes Study: Effect on Erectile Function, Penile Sensitivity, Sexual Activity and Satisfaction. J Urol. 2002; 167(5): 2113-6.
- ↑
 Van Howe RS. Incidence of meatal stenosis following neonatal circumcision in a primary care setting. Clin Pediatr (Phila). January 2006; 45(1): 49-54. Retrieved 15 December 2019.
Van Howe RS. Incidence of meatal stenosis following neonatal circumcision in a primary care setting. Clin Pediatr (Phila). January 2006; 45(1): 49-54. Retrieved 15 December 2019.
- ↑
 Stenram A, Malmfors G, Okmian L. Circumcision for phimosis: a follow-up study. Scandinavian journal of urology and nephrology. 1986; 20(2): 89. PMID.
Stenram A, Malmfors G, Okmian L. Circumcision for phimosis: a follow-up study. Scandinavian journal of urology and nephrology. 1986; 20(2): 89. PMID.
- ↑

Meatal Stenosis
, Medscape. Retrieved 11 October 2019. - ↑
 Park JK, Doo AR, Kim JH, Park HS, et al. Prospective investigation of penile length with newborn male circumcision and second to fourth digit ratio.. Can Urol Assoc J. September 2016; 10(9-10) PMID. PMC. DOI. Retrieved 4 September 2022.
Park JK, Doo AR, Kim JH, Park HS, et al. Prospective investigation of penile length with newborn male circumcision and second to fourth digit ratio.. Can Urol Assoc J. September 2016; 10(9-10) PMID. PMC. DOI. Retrieved 4 September 2022.
- ↑
 Winkelmann RK. The erogenous zones: their nerve supply and significance. Mayo Clin Proc. 21 January 1959; 34(3): 39-47. PMID. Retrieved 4 June 2021.
Winkelmann RK. The erogenous zones: their nerve supply and significance. Mayo Clin Proc. 21 January 1959; 34(3): 39-47. PMID. Retrieved 4 June 2021.
- ↑
 Van Howe RS, Cold CJ. Advantages and Disadvantages of Neonatal Circumcision. The Journal of the American Medical Association. 2 April 1997; 277(13): 1052-7. PMID.
Van Howe RS, Cold CJ. Advantages and Disadvantages of Neonatal Circumcision. The Journal of the American Medical Association. 2 April 1997; 277(13): 1052-7. PMID.
- ↑
 Marshall RE, Porter FL, Rogers AG, et al. Circumcision: II effects upon mother-infant interaction. Early Hum Dev. 1982; 7(4): 367-74. Retrieved 1 February 2020.
Marshall RE, Porter FL, Rogers AG, et al. Circumcision: II effects upon mother-infant interaction. Early Hum Dev. 1982; 7(4): 367-74. Retrieved 1 February 2020.
- ↑
 Ramos S, Boyle GJ (2001):
Ramos S, Boyle GJ (2001): Ritual and medical circumcision among Filipino boys: evidence of post-traumatic stress disorder
, in: Understanding circumcision: A Multi-Disciplinary Approach to a Multi-Dimensional Problem. George C. Denniston, Frederick M. Hodges, Marilyn Fayre Milos (eds.). New York: Kluwer Academic/Plenum Publishers. Pp. 253-70. - ↑ a b

Global Survey of Circumcision Harm
. Retrieved 12 October 2019. - ↑
 van der Kolk BA. The compulsion to repeat the trauma: re-enactment, revictimization, and masochism. Psychiatr Clin North Am. June 1989; 12(2): 389-411. PMID. Retrieved 10 November 2022.
van der Kolk BA. The compulsion to repeat the trauma: re-enactment, revictimization, and masochism. Psychiatr Clin North Am. June 1989; 12(2): 389-411. PMID. Retrieved 10 November 2022.
- ↑
 Goldman R. The psychological impact of circumcision. BJU Int. 1999; 83(Suppl. 1): 93-103. Retrieved 12 October 2019.
Goldman R. The psychological impact of circumcision. BJU Int. 1999; 83(Suppl. 1): 93-103. Retrieved 12 October 2019.
- ↑
 Rhinehart J. Neonatal circumcision reconsidered. Transactional Analysis J. 1999; 29(3): 215-21. Retrieved 12 October 2019.
Rhinehart J. Neonatal circumcision reconsidered. Transactional Analysis J. 1999; 29(3): 215-21. Retrieved 12 October 2019.
- ↑
 Cansever G. Psychological effects of circumcision. Brit. J. Med. Psychol. 1965; 38: 321-31. Retrieved 12 October 2019.
Cansever G. Psychological effects of circumcision. Brit. J. Med. Psychol. 1965; 38: 321-31. Retrieved 12 October 2019.
- ↑ a b c
 Levy DM. Psychic trauma of operations in children; and a note on combat neurosis. American Journal of Diseases of Children. 1945; 69: 7-25. Retrieved 12 October 2019.
Levy DM. Psychic trauma of operations in children; and a note on combat neurosis. American Journal of Diseases of Children. 1945; 69: 7-25. Retrieved 12 October 2019.
- ↑
 Bollinger, Dan / Georganne Chapin: Child genital cutting as an adverse childhood experience
Bollinger, Dan / Georganne Chapin: Child genital cutting as an adverse childhood experience  , Intact America (Tarrytown). (August 2019). Retrieved 2 November 2021.
, Intact America (Tarrytown). (August 2019). Retrieved 2 November 2021.
- ↑ a b
 Bollinger D, Boy's Health Advisory. Lost Boys: An Estimate of U.S. Circumcision-Related Infant Deaths. Thymos: Journal of Boyhood Studies. 26 April 2010; 4(1): 78-90. DOI. Retrieved 12 October 2019.
Bollinger D, Boy's Health Advisory. Lost Boys: An Estimate of U.S. Circumcision-Related Infant Deaths. Thymos: Journal of Boyhood Studies. 26 April 2010; 4(1): 78-90. DOI. Retrieved 12 October 2019.
- ↑
 (26 April 2010).
(26 April 2010). Infant circumcision causes 100 deaths each year in US
, International Coalition for Genital Integrity, ICGI. - ↑ For example, Frederick M. Hodges, a medical historian, writes: "In the late 1970s, as the Americans were growing increasingly aware of the abuses of power rampant throughout the nation's social institutions, influential grass-roots movements protesting the forced circumcision of American children sprang up nationwide." F. Hodges, "A Short History," p. 31; see also Glick, Marked in Your Flesh, pp. 273-281.
- ↑
 Fletcher CR (1999):
Fletcher CR (1999): Section 5
, in: Circumcision in America in 1998: Attitudes, Beliefs, and Charges of American Physicians. Work: Male and Female Circumcision. George C. Denniston, Frederick M. Hodges, Marilyn Fayre Milos (eds.). New York: Kluwer Academic/Plenum Publishers. Pp. 259-71. Retrieved 12 October 2019.
Note: ID 10.1007/978-0-585-39937-9_19 - ↑ See, e.g., Shephard and Shephard, The Complete Guide, p. 125.
- ↑ Lannon and Bailey, "Circumcision Policy Statement," p. 691.
- ↑
 Re J (child's religious upbringing and circumcision). Family Court Reports. 2000; 1: 307-14. Retrieved 12 October 2019.
Re J (child's religious upbringing and circumcision). Family Court Reports. 2000; 1: 307-14. Retrieved 12 October 2019.
- ↑ See, e.g., Somerville, "Therapeutic and Non-Therapeutic Medical Procedures"; Poulter, English Criminal Law; Chessler, "Justifying the Unjustifiable"; Smith, "Male Circumcision."
- ↑
 Hill G. The case against circumcision. Journal of Men's Health and Gender. 2007; 4(3): 318-23. Retrieved 30 May 2021.
Hill G. The case against circumcision. Journal of Men's Health and Gender. 2007; 4(3): 318-23. Retrieved 30 May 2021.
- ↑
 MacNeily, Andrew. Routine circumcision: the opposing view. Can Urol Assoc J. November 2007; 1(4): 395-7. PMID. DOI. Retrieved 8 November 2021.
MacNeily, Andrew. Routine circumcision: the opposing view. Can Urol Assoc J. November 2007; 1(4): 395-7. PMID. DOI. Retrieved 8 November 2021.
- ↑
 Non-therapeutic circumcision of male minors
Non-therapeutic circumcision of male minors  , Royal Dutch Medical Association. (2010). Retrieved 8 November 2021.
, Royal Dutch Medical Association. (2010). Retrieved 8 November 2021.
- ↑
 Circumcision of Infant Males
Circumcision of Infant Males  , The Royal Australasian College of Physicians. (1 September 2010). Retrieved 8 November 2021.
, The Royal Australasian College of Physicians. (1 September 2010). Retrieved 8 November 2021.
- ↑
 Darby R. To avoid circumcision complications, avoid circumcision. Can Urol Assoc J. 14 August 2014; 8(7-8): 231. DOI. Retrieved 16 December 2022.
Darby R. To avoid circumcision complications, avoid circumcision. Can Urol Assoc J. 14 August 2014; 8(7-8): 231. DOI. Retrieved 16 December 2022.
- ↑
 Sorokin ST, Finlay, JC, Jeffries, AL, et al. Newborn male circumcision. Paediatr Child Health. August 2015; 20(6): 311-20. PMID. PMC. DOI. Retrieved 27 October 2019.
Sorokin ST, Finlay, JC, Jeffries, AL, et al. Newborn male circumcision. Paediatr Child Health. August 2015; 20(6): 311-20. PMID. PMC. DOI. Retrieved 27 October 2019.
- ↑
 Dave S, et al. Canadian Urological Association guideline on the care of the normal foreskin and neonatal circumcision in Canadian infants (abridged version). Can Urol Assoc J. February 2018; 12(2): 18-28. Retrieved 9 November 2021.
Dave S, et al. Canadian Urological Association guideline on the care of the normal foreskin and neonatal circumcision in Canadian infants (abridged version). Can Urol Assoc J. February 2018; 12(2): 18-28. Retrieved 9 November 2021.
- ↑
 Committee on Bioethics, American Academy of Pediatrics. Informed consent, parental permission, and assent in pediatric practice. Pediatrics. 1995; 95(2): 314-17. PMID. Retrieved 21 May 2023.
Committee on Bioethics, American Academy of Pediatrics. Informed consent, parental permission, and assent in pediatric practice. Pediatrics. 1995; 95(2): 314-17. PMID. Retrieved 21 May 2023.
- ↑
 Committee on Bioethics. Informed Consent in Decision-Making in Pediatric Practice
Committee on Bioethics. Informed Consent in Decision-Making in Pediatric Practice  . Pediatrics. August 2016; 138(2): e20161485. PMID. DOI. Retrieved 21 May 2023.
. Pediatrics. August 2016; 138(2): e20161485. PMID. DOI. Retrieved 21 May 2023.
- ↑
 Committee on Bioethics. Informed Consent in Decision-Making in Pediatric Practice
Committee on Bioethics. Informed Consent in Decision-Making in Pediatric Practice  . Pediatrics. August 2016; 138(2): e20161484. PMID. DOI. Retrieved 21 May 2023.
. Pediatrics. August 2016; 138(2): e20161484. PMID. DOI. Retrieved 21 May 2023.
- ↑
 Myers A, Earp BD. What is the best age to circumcise? A medical and ethical analysis. J Biosoc Sci. September 2020; 34(7): 560-72. PMID. DOI. Retrieved 18 May 2023.
Myers A, Earp BD. What is the best age to circumcise? A medical and ethical analysis. J Biosoc Sci. September 2020; 34(7): 560-72. PMID. DOI. Retrieved 18 May 2023.